 Are you struggling to understand the intricacies of Medicare supplement underwriting? You’re not alone. Navigating the insurance world can be daunting, but fear not – we’ve got you covered. In this medicare supplement underwriting cheat sheet, we’ll unlock the secrets of insurance underwriting for Medigap policies. We’ll make it easier for you to understand and find the coverage that meets your needs.
Are you struggling to understand the intricacies of Medicare supplement underwriting? You’re not alone. Navigating the insurance world can be daunting, but fear not – we’ve got you covered. In this medicare supplement underwriting cheat sheet, we’ll unlock the secrets of insurance underwriting for Medigap policies. We’ll make it easier for you to understand and find the coverage that meets your needs.
Whether you’re new to Medicare or have been enrolled for years, underwriting can be confusing. But it doesn’t have to be. We’ll break down the process step-by-step, explaining the factors that insurers consider when determining your eligibility and pricing for Medicare supplement plans. From medical history and pre-existing conditions to age and location, we’ll leave no stone unturned.
Armed with this knowledge, you’ll be better equipped to navigate the Medicare supplement landscape and make informed decisions about your coverage. So, grab your pen and paper, and let’s create your own Medicare Supplement underwriting cheat sheet together. By the end of this cheat sheet, you’ll feel confident and empowered to take control of your healthcare coverage.
Develop Your Own Cheat Sheet for Medicare Supplement Insurance & Underwriting
Medicare supplement insurance, also known as Medigap, is designed to fill the gaps in original Medicare coverage. While original Medicare covers many healthcare expenses, it doesn’t cover everything.
Part A currently has a hospital deductible of $1,632 per event in a 60-day period, and Part B has an unlimited 20% coinsurance. That’s why you need a Medicare supplement policy to fill in the gaps.
Private insurance companies offer these policies to help you pay out-of-pocket costs such as deductibles, copayments, and coinsurance. How do you get a Medicare Supplement policy?
The Basics of Insurance Underwriting
During your Initial Enrollment Period into Medicare, the insurance company is required to sell you a Medicare Supplement without asking any health questions–underwriting. After your one-time Initial Enrollment Period into Medicare, you will need to answer health questions and pass underwriting to purchase a Medicare Supplement in most states.
Underwriting is the process insurance companies use to assess an applicant’s risk and determine eligibility for coverage. When it comes to Medicare supplement insurance, underwriting plays a crucial role in determining whether you’ll be approved for a plan and how much you’ll pay in premiums.
When people are denied during underwriting or rated, they are usually not happy. Some people are even upset and offended. I understand. I get rated as obese myself under most insurance underwriting. I’ve been lifting weights since I was twelve, so there is plenty of muscle. But guess what? My body fat is not 6%, either, so I’m fat. So, I pay more. I am working hard on trying to grow taller for my weight category. So far, it has yet to work.
Of course, the people who pass underwriting are happy, but they should be happy because others were not allowed into their insurance pool. Because a certain level of health is required, the number of clients can be covered with an affordable amount of premium. You want as low a number of claims as possible because that keeps your premiums low. The same goes for car insurance, homeowners insurance, and boat insurance. When there is a natural disaster, like hail or hurricanes, that is why premiums usually go up afterward.
Sometimes, actuaries get the underwriting wrong because insurance companies WANT to insure more people. The more people they insure; the more money they make usually–if they do it correctly.
When they do it incorrectly–in other words, poor underwriting standards–the result is that people with potential health issues get into the pool. There are more claims than what the actuaries planned for, and the insurance company must make up the difference by increasing premiums for everyone.
Why Underwriting is Important in Medicare Supplement Insurance
Underwriting is necessary in Medicare supplement insurance because it helps companies manage risk. By assessing an applicant’s health status and other factors, insurers can determine the likelihood of the individual filing claims and estimate the potential costs they may incur. This allows them to set appropriate premiums that reflect the risk level the insurance company is taking on.
 Factors Considered in Medicare Underwriting
Factors Considered in Medicare Underwriting
Here is the meat of what you are looking for. During the underwriting process for Medicare supplement insurance, several factors are taken into consideration. These factors can vary slightly depending on the insurance company, but some common ones include:
1. Age: Younger individuals may be seen as lower risk than older individuals with more health issues.
2. Gender: Although gender-based pricing is not allowed in some states, it may still be a factor in underwriting. In Nebraska & Iowa, Medicare Supplements are priced based on gender, and men are always more expensive.
3. Location: The area where you live can impact the cost of healthcare and, therefore, affect underwriting decisions.
I mainly do Medicare insurance in Nebraska and Iowa. I’m amazed at the price differences between Nebraska and Iowa, Omaha and Lincoln, and urban and rural areas. Ultimately, some areas are healthier than others and consequently have fewer claims. Thus the premiums are lower.
4. Medical history: Insurance companies will review an applicant’s medical history to assess pre-existing conditions and potential risks. As part of the application process, you give the insurance company permission to access various insurance resources that give a history of your health. You list your current medications and the dosage on the application. Medications tell a great deal about your health profile.
5. Tobacco use: Smokers may face higher premiums due to the increased health risks associated with smoking. Some companies do not count you as a smoker during your Initial Enrollment Period into Medicare. We definitely highlight these companies to our new clients who are smokers.
6. Enrollment period: The timing of your application can impact underwriting decisions, as there are specific enrollment periods where guaranteed issue rights apply. This particular issue is NOT relevant to Medicare supplements in Nebraska and Iowa. There are no special periods, like the birthday or anniversary rule.
Common Underwriting Requirements
Insurance companies may require applicants to go through underwriting when applying for Medicare supplement insurance. The underwriting requirements can include:
Medical Underwriting
This involves answering health-related questions on the application form. People always ask if there is a physical; there is no physical. The health questions only take 5-8 minutes to answer. The medical side of underwriting is all done electronically. In a moment, insurance companies can scan your medical records and prescriptions to make a determination. Some companies have the whole process so automated that I get an answer within seconds.
Pre-existing Conditions
Insurance companies may ask about pre-existing conditions and impose waiting periods or exclusions for specific conditions. For example, most health questions begin with a qualifier: “In the past two years . . . .” “In the last six months . . . .” “Do you take _____ amount of insulin?”
Just because you had cancer in the past, a heart attack in the past, or a stroke in the past, you are NOT automatically disqualified. The bigger questions is how longer go did it occur, what has been your health since, and was the problem rectified?
Guaranteed Issue Rights
There are specific situations where insurance companies must offer coverage without underwriting, such as when an individual is losing other health coverage. There are restrictions; for example, you can only select Plan G.
Medicare regulations in Nebraska and Iowa only have a Medicare guarantee issue for when you lose an employer health plan and are on Medicare. Nebraska & Iowa do not have a Medicare Supplement Open Enrollment.
How Medicare Underwriting Impacts Premium Rates
Underwriting can significantly impact the premium rates you’ll pay for your Medicare supplement insurance. Based on the information gathered during the underwriting process, insurance companies determine the level of risk you represent and adjust your premiums accordingly. If you’re considered a higher risk, you may face higher premiums, while lower-risk individuals may enjoy more affordable rates. In some cases, the risk is too high, and the company denies coverage.
Implement Your Medicare Supplement Underwriting Cheat Sheet
Navigating the underwriting process for Medicare supplement insurance can seem daunting, but by developing your own medicare supplement underwriting cheat sheet, you can increase your chances of success.
Research and Compare Plans
Before applying, research and compare different Medicare supplement plans to find the one that best suits your needs. We do hundreds of Medicare Supplement applications a year. We know the companies that are strict or more lenient. Some companies will cover insulin-dependent diabetics; many will not. We know the levels of A1C that are acceptable to some insurance companies and will be rejected by others. Rheumatoid arthritis is immediately rejected by some companies but is allowable under certain circumstances by others. Each company picks its segment of the market it wants to go after and specialize in. We help our clients find the needle in the haystack.
Understand the Underwriting Process.
Familiarize yourself with the underwriting requirements of different insurance companies so you know what to expect during the application process. Understanding the process may be as simple as losing a few pounds. That will get you into a better health class and a lower premium.
Adjust your diet and then visit your doctor to have your blood tested. Reduced cholesterol or A1C levels may be enough to push you into the next underwriting category.
Be Honest and Accurate.
Provide truthful and accurate information on your application to avoid any complications or potential issues later on. They will know if you are a smoker. You will not be able to avoid the smoking rate by not disclosing tobacco use, even chewing.
Seek Professional Assistance
If you’re unsure about the underwriting process or need help with your application, consider contacting a licensed insurance agent professional or broker specializing in Medicare supplement insurance.
At Omaha Insurance Solutions, we know the landscape of Medicare Supplements in Nebraska and Iowa. We can direct you to the plan that will be most favorable to your health circumstances and budget, especially if you have some health challenges. Insurance professionals do not cost you anything. The price is exactly the same if you do all the work yourself or use an insurance agent. Why not use someone who has a thorough knowledge of the plans in your area? Give us a call at 402-614-3389.
Common Underwriting Mistakes to Avoid
When going through the underwriting process for Medicare supplement insurance, it’s essential to avoid common mistakes that could potentially lead to application denials or higher premiums.
Providing incorrect information
Ensure that all the information you provide on your application is accurate and current.
I have clients who are “too honest.” They think if they explain and justify certain health issues, the insurance company will understand and forgive. In my experience, when the underwriter hears certain words and phrases, they sometimes overreact. As scientific as they try to make it, underwriting is still a very human process. It is the job of the underwriter to protect the insurance company. We then have to contact the doctors and go through a difficult and lengthy process to explain the health situation so the person is passed through underwriting.
underwriting is still a very human process. It is the job of the underwriter to protect the insurance company. We then have to contact the doctors and go through a difficult and lengthy process to explain the health situation so the person is passed through underwriting.
My recommendation is like Sergeant Joe Friday used to say, “Just the facts, mam, just the facts.”
Failing to disclose pre-existing conditions
Be thorough when disclosing any pre-existing conditions, as failure could result in coverage denial or exclusions. They will find everything. I guarantee.
Where this situation becomes sticky is with surgeries. One of the questions that is on every application is: “Has a medical professional recommended you have any surgical procedures?” Or, “Do you have any medical procedures scheduled, such as cataract, joint replacement, or hip replacement surgery?” Or words to that effect.
The new insurance company does not want to get stuck with a surgical bill that should go to the existing insurance provider. After the surgery is completed and you are fully recovered, then you can proceed along with the application.
If you are not forth coming with that information and you do have a surgical procedure done after going on the new policy, like cataract surgery, the insurance company is in a position to say that you were not honest on the application. Then they will deny the claim. You will then be responsible for the full cost out of your pocket.
Honesty Is the Best Policy
Over the years, I have had prospective clients not disclose important information, “forget,” or lie. “I forgot the doctor said I have a mild case of Alzheimer’s.” “I only smoke once in a while.” “The cancer is really slow growing. The doctor said it’s tiny.” “I didn’t know it was COPD. I thought it was bad asthma.”
While I’m sympathetic to harsh medical circumstances and the desire to reduce insurance costs, it doesn’t alter the reality they will not be offered a new Medicare Supplement. The whole endeavor ends up being a waste of time for everyone involved.
Fortunately, systems are in place where insurance companies are almost infallible in finding out medical history. That is a good thing because if a policy were issued under materially false circumstances, the person who made false or misleading claims would be in serious financial hazard. The process protects everyone involved.
Not Reviewing Your Application
Review it carefully before submitting it to ensure all the information is correct and complete. When an application is denied by an insurance company, there is a record.  Even if there was a mistake made in the application process, it is not as simple as reapplying with the same insurance company or another. Depending on the situation, the person may be prevented from reapplying for several months.
Even if there was a mistake made in the application process, it is not as simple as reapplying with the same insurance company or another. Depending on the situation, the person may be prevented from reapplying for several months.
 How to Improve Your Chances of Approval
How to Improve Your Chances of Approval
While the underwriting process for Medicare supplement insurance can be strict, there are steps you can take to improve your chances of approval:
1. Maintain good health: Adopt a healthy lifestyle and manage any existing health conditions to demonstrate that you are a lower risk.
2. Consider alternative plans: If you’re facing difficulties with underwriting, explore alternative options, such as Medicare Advantage plans, which may have less stringent underwriting requirements.
3. Seek professional guidance: If you need clarification on the underwriting process or assistance with your application, consult a licensed insurance agent or broker who can provide tailored guidance.
Bottom Line: Mastering Medicare Supplement Underwriting
Navigating the world of Medicare supplement underwriting doesn’t have to be overwhelming. By understanding the basics of underwriting, the factors considered, and the common mistakes to avoid, you’ll develop your own medicare supplement underwriting cheat sheet. Research different plans, gather necessary documentation, and seek professional guidance. With these tools, you will have a checklist to go through during the underwriting process and find the Medicare supplement plan that best meets your needs. So, take control of your healthcare coverage and unlock the secrets of Medicare supplement underwriting by building your own cheat sheet.
Get Your Own Expert Medicare Underwriting Guide
At Omaha Insurance Solutions, we are happy to share with you our wealth of knowledge & experience with Medicare Supplement underwriting. Our Medicare Supplement underwriting cheat sheet was developed over a

Christopher J. Grimmond, MA, CFP
decade with thousands of clients. We have learned the lessons of Medicare Supplement underwriting.
The cost is EXACTLY the same whether you use an insurance agent or call the insurance company directly. The difference with us is you see all of the insurance companies and Medicare Supplements, not just one or two.
Our loyalty is to our clients, not to an insurance company. We can change companies on a dime.
And when your cost goes up, we are not going to say keep the policy. We are going to look for the same coverage with a solid A-rated company at a lower cost. If you can call the insurance company you have your policy with, I guarantee they will not recommend another insurance company.
We know the subtleties of the underwriting process and which company will be most favorable to your health situation. Not all companies are created equal, and we have learned the hard way over the years which ones to trust. You’ll get that experience with us.
Over the years, we’ve learned a thing or two about Medicare Supplements and underwriting. We also take care of all the paperwork, follow-up, and headaches that come with dealing with an insurance company. Call us for a free consultation at 402-614-3389.
 Are you looking to maximize your healthcare coverage? In this article, we will explain the benefits of Medicare Advantage Part C, helping you make informed decisions about your healthcare options. Medicare Advantage Part C offers an alternative to traditional Medicare coverage, providing additional benefits and services to enhance your overall healthcare experience.
Are you looking to maximize your healthcare coverage? In this article, we will explain the benefits of Medicare Advantage Part C, helping you make informed decisions about your healthcare options. Medicare Advantage Part C offers an alternative to traditional Medicare coverage, providing additional benefits and services to enhance your overall healthcare experience.
With Medicare Advantage Part C, you can enjoy prescription drug coverage, vision and dental care, and even fitness programs. These additional services can save you money and provide comprehensive coverage tailored to your specific needs.
But how do you know if Medicare Advantage Part C is correct for you? We’ll explore the eligibility criteria and factors to consider when weighing your options. Understanding the ins and outs of Medicare Advantage Part C will empower you to make the best choice for your healthcare needs.
So, if you’re ready to take control of your healthcare coverage and get the most out of your benefits, keep reading. Let’s dive into the Medicare Advantage Part C world and discover the possibilities it holds for you.
Understanding the Basics of Medicare Advantage Part C Benefits
Medicare Advantage Part C, also known as Medicare Advantage Plans, is a comprehensive healthcare option offered by private insurance companies approved by Medicare. It combines the benefits of Medicare Parts A & B, and usually Part D, as well as additional services and coverage options. Medicare Advantage Part C is managed care, which means it is a network system. Doctors, hospitals, and clinics contract with the insurance company.
One of the key advantages of Medicare Advantage Part C is that it often includes prescription drug coverage, known as Medicare Part D, which is not included in Original Medicare. This means you can cover all your healthcare needs, including medications, under a single plan. Additionally, many Medicare Advantage plans offer extra benefits such as vision and dental care, hearing aids, and even fitness programs to help you stay healthy and active.
But how do you know if Medicare Advantage Part C is right for you? Let’s explore the eligibility criteria and factors when weighing your options.
The Benefits of Medicare Advantage Part C
Medicare Advantage Part C offers a wide range of benefits that can significantly enhance your healthcare coverage. These benefits can include:
include:
- Comprehensive coverage: Medicare Advantage Part C combines the benefits of Medicare Parts A and B, providing hospital insurance (Part A) and medical insurance (Part B) in one plan. This means you have coverage for hospital stays, doctor visits, preventive care, and more.
- Prescription drug coverage: Many Medicare Advantage plans include prescription drug coverage, allowing you to obtain your medications conveniently through the same plan. This can save you money and reduce the hassle of managing multiple insurance providers.
- Additional services: Medicare Advantage Part C plans often offer additional services not covered by Original Medicare, such as vision and dental care, hearing aids, and wellness programs. These services can help you maintain your overall health and well-being.
- Out-of-pocket cost protection: Medicare Advantage plans have a cap on out-of-pocket expenses, providing financial protection in case of unexpected medical costs. This can bring peace of mind and help you plan your healthcare budget more effectively.
How to Qualify for Part C
 To be eligible for Medicare Advantage Part C, you must meet the following requirements:
To be eligible for Medicare Advantage Part C, you must meet the following requirements:
- Enrollment in Medicare Parts A and B: You must be enrolled in both Medicare Part A (hospital insurance) and Part B (medical insurance) to be eligible for Medicare Advantage Part C.
- Residency: You must reside in the service area of the Medicare Advantage plan you wish to join. Residency is important to remember. I have had clients move without telling me or the plan. They are then surprised when their coverage doesn’t work or is even canceled.
It’s important to note that eligibility requirements may vary depending on the specific Medicare Advantage plan and insurance provider. There are special needs plans for those on state Medicaid or with chronic health conditions like diabetes, COPD, or heart disease. These plans have additional requirements.
Review the requirements and seek guidance from a qualified insurance agent to ensure you meet the eligibility criteria. These plans have even richer benefits for those who qualify.
Differences Between Original Medicare Vs. Medicare Advantage
While Original Medicare and Medicare Advantage Part C both provide healthcare coverage, there are some key differences between the two:
- Coverage options: Original Medicare consists of Part A (hospital insurance) and Part B (medical insurance), while Medicare Advantage Part C combines both Parts A and B into a single plan. Medicare Advantage plans also often include additional benefits, such as prescription drug coverage and extra services.
- Network restrictions: Original Medicare allows you to go to any doctor or hospital that accepts Medicare, while Medicare Advantage plans typically have a network of providers you must use to receive full coverage. However, some Medicare Advantage plans offer out-of-network coverage for higher out-of-pocket costs.
- Cost structure: Original Medicare deductibles and coinsurance have no cap or maximum out-of-pocket. Many purchase
 additional coverage—a Medigap plan—to cover the significant gaps in coverage. This additional insurance comes at an additional cost. Medicare Advantage has minimal copays with a maximum out-of-pocket as well as additional benefits. Most of the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs area have zero monthly premium. You simply continue to pay your Medicare Part B premium, which you are paying anyway.
additional coverage—a Medigap plan—to cover the significant gaps in coverage. This additional insurance comes at an additional cost. Medicare Advantage has minimal copays with a maximum out-of-pocket as well as additional benefits. Most of the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs area have zero monthly premium. You simply continue to pay your Medicare Part B premium, which you are paying anyway. - Flexibility: Original Medicare allows you to see any specialist or visit any healthcare provider without a referral. While some Medicare Advantage HMO plans in other parts of the country require referrals to see specialists, the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs areas are open access. Open Access means you can see any specialist in the network without a referral.
Considering these differences can help you determine which type of coverage aligns best with your healthcare needs and preferences.
Choosing the Right Medicare Advantage Part C Plan
 Choosing the right Medicare Advantage Part C plan requires careful consideration of your healthcare needs and personal preferences. Here are some factors to consider when selecting a plan:
Choosing the right Medicare Advantage Part C plan requires careful consideration of your healthcare needs and personal preferences. Here are some factors to consider when selecting a plan:
- Coverage and benefits: Review the coverage options and benefits offered by different Medicare Advantage plans. Consider your specific healthcare needs, such as prescription drugs, vision, and dental care, or fitness programs, and choose a comprehensive plan for your requirements.
- Provider network: Check whether the plan’s network includes your preferred doctors, hospitals, and specialists. Ensure the plan’s network is convenient and accessible for your healthcare needs. All four networks work with the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs areas. If the provider is part of CHI, Nebraska Medicine, Methodist Health Systems, or Bryan Health, they will be in the network.
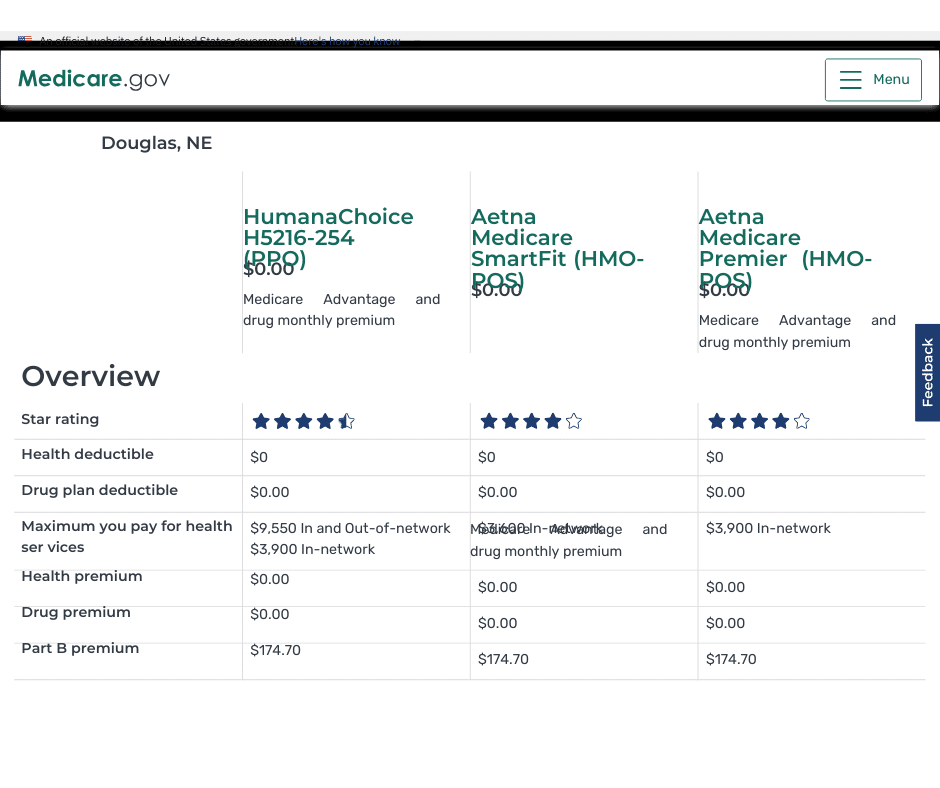
- Costs: Compare the costs associated with different Medicare Advantage plans, including monthly premiums, deductibles, copayments, and coinsurance. Consider your budget and evaluate which plan offers the most cost-effective coverage for your needs.
I recommend starting with the maximum out-of-pocket (MOOP) amount and the star rating. Maximum out-of-pocket is what you have at risk. The star rating can help you narrow down the plans that have been around for a while and have a good service record.
Researching and comparing different Medicare Advantage plans can help you select the best plan that aligns with your healthcare needs and budget. At Omaha Insurance Solutions, we help clients evaluate the universe of Medicare plans quickly & easily using our sophisticated but user-friendly software, and with over a decade of experience, we know the local Medicare plans intimately.
Exploring Additional Benefits
Medicare Advantage Part C plans often provide additional benefits that go beyond what Original Medicare offers. These benefits can vary depending on the specific plan and insurance provider, but commonly include:
- Vision and dental care: Many Medicare Advantage plans cover routine vision and dental services, including exams,
 cleanings, and eyeglasses.
cleanings, and eyeglasses. - Hearing aids: Some plans offer coverage for hearing aids and related services, helping you maintain your hearing health.
- Fitness programs: Medicare Advantage plans may provide access to fitness programs, gym memberships, or wellness classes to help you stay active and improve your overall health. I belong to the Genesis Health Clubs in Omaha. My membership is almost $600 a year. I would be very happy to have my health insurance plan pay that fee. I’m looking forward to Medicare. In the Silver Sneakers and Renew Active Programs, you can actually join multiple gyms. You are not limited to one chain or a single club.
- Transportation services: Certain plans offer transportation services to and from medical appointments, ensuring you can get the care you need even if you don’t have reliable transportation.
These additional benefits can significantly enhance your healthcare experience and provide you with comprehensive coverage tailored to your specific needs. Original Medicare does not provide these benefits. If you want additional benefits, you must purchase them at additional costs.
 Common Misconceptions about Medicare Advantage Part C
Common Misconceptions about Medicare Advantage Part C
There are several misconceptions surrounding Medicare Advantage Part C. Let’s address some of the most common ones:
- Limited provider choice: While provider networks are not an issue with the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs areas, it certainly may be a concern in other places. There are typically, however, many options to choose from within most networks. Additionally, some plans offer out-of-network coverage for higher out-of-pocket costs.
- Lack of coverage for pre-existing conditions: Medicare Advantage plans cannot deny coverage based on pre-existing conditions. They must cover all services covered by Original Medicare, even if you have a pre-existing condition.
- Difficulty changing plans: Medicare beneficiaries have the opportunity to change their Medicare Advantage plans during the Annual Enrollment Period, which typically occurs from October 15th to December 7th each year. They also have a second opportunity during the Open Enrollment Period, which occurs from January 1st to March 31st, to make a one-time change to a Medicare Advantage plan.
- Higher costs: While Medicare Advantage plans have copays and coinsurance, these copays are generally small and have a cap. Medigap plans have a monthly cost that increases with age and usually exceeds annual copays on Medicare Advantage plans most of the time in most years.
Understanding these misconceptions can help you make informed decisions about Medicare Advantage Part C and ensure you have accurate information when considering your healthcare options.
Tips for Maximizing Your Medicare Advantage Part C Benefits
To make the most of your Medicare Advantage Part C benefits, consider the following tips:
- Review your plan annually: Medicare Advantage plans can change their coverage and benefits each year. Take the time to review your plan’s Annual Notice of Change (ANOC) to ensure it still meets your healthcare needs. Check the cost of medications for the coming year. We offer an annual review to our clients. However, some clients ignore our letters, emails, and phone calls to meet. We get distressed calls in the new year when plan changes catch up with some folks.
- Stay within your plan’s network: To receive full coverage and avoid higher out-of-pocket costs, use healthcare providers within your plan’s network. If you need to see a specialist or receive services outside the network, consult your plan’s guidelines for appropriate referrals or prior authorization. As I said earlier, this is generally not an issue in our area with doctors and hospitals; problems can arise with dentists and optimists who are not within the network. Double-check with the network because providers do change who they work with.
- Take advantage of additional benefits: Explore the extra benefits offered by your Medicare Advantage plan, such as vision and dental care or fitness programs. Utilizing these services can help you stay healthy and maximize the value of your plan. These Medicare Advantage Part C benefits save you money. I’m surprised when clients don’t utilize the over-the-counter benefit. In some cases, that is hundreds of dollars not coming out of your pocket.
- Understand your costs: Familiarize yourself with your plan’s copayments, deductibles, and coinsurance to avoid unexpected expenses. Knowing your costs upfront can help you budget for healthcare expenses more effectively. I always recommend clients talk with the doctor’s back office before any procedure is performed. Make sure the office received any prior approvals and find out the approximate cost to you beforehand so there are no surprises.
Following these tips can optimize your healthcare coverage and ensure you get the most out of your Medicare Advantage Part C plan.
Bottom Line: Making the Most of your Medicare Advantage Part C Benefits
Medicare Advantage Part C offers a comprehensive and flexible alternative to traditional Medicare coverage. With additional benefits such as prescription drug coverage, vision and dental care, and fitness

Christopher J. Grimmond, MA, CFP
programs, Medicare Advantage plans can provide you with comprehensive coverage tailored to your specific needs. Understanding the basics of Medicare Advantage Part C, eligibility criteria, and differences from Original Medicare is crucial in making informed decisions about your healthcare options.
By choosing the right Medicare Advantage Part C plan, exploring additional benefits, and maximizing your coverage, you can take control of your healthcare and enjoy comprehensive and cost-effective coverage.
If you’re ready to maximize your healthcare coverage and get the most out of your benefits, consider exploring the possibilities of Medicare Advantage Part C. Take charge of your healthcare journey today. Give us a call at Omaha Insurance Solutions at 402-614-3389 to view the Medicare Advantage Part C plans you are eligible for in your area to ensure a healthier and more secure future.
 Is it overwhelming to choose the best Medicare plan for your needs? With so many options available, it’s understandable. But worry not because we have your ultimate solution – the Medicare Plan Comparisons Chart.
Is it overwhelming to choose the best Medicare plan for your needs? With so many options available, it’s understandable. But worry not because we have your ultimate solution – the Medicare Plan Comparisons Chart.
The best way to compare is side-by-side. We can see each relevant benefit or cost in chart form and compare apples to apples. There is still a lot of information to comb through and remember, but a chart helps to reduce some of the confusion and the mental work of remembering what each Medicare plan offers.
Whether you’re looking for a plan that covers prescription drugs, outpatient surgeries, or dental more favorably, you can look at your options in the Medicare plan comparison chart.
By utilizing this user-friendly chart, you can easily compare different plans side by side, evaluate their features and benefits, and make an informed decision based on your unique healthcare needs.
Choosing the right Medicare plan is crucial because it directly impacts your overall health and pocketbook. At Omaha Insurance Solutions, we aim to simplify your Medicare selection process by providing all the necessary information in one place. With a Medicare Plan Comparisons Chart, you can confidently select the plan that meets your specific requirements and enjoy peace of mind knowing that you have made the best choice for your healthcare coverage.
Understanding Medicare Plans
Medicare is a federal health insurance program that provides coverage for individuals aged 65 and older and younger individuals with certain disabilities. It consists of different parts, each covering specific services and treatments.
To understand which Medicare plan is best for you, it’s essential to familiarize yourself with the different types of plans available and their respective coverage options. This knowledge will enable you to make an informed decision based on your healthcare needs.
Types of Medicare Plans
There are four main types of Medicare plans: Original Medicare (Part A and Part B), Medicare Advantage (Part C), Medicare Supplement Insurance (Medigap), and Prescription Drug Coverage (Part D).
- Original Medicare (Part A and Part B): This is the traditional Medicare plan offered by the government. Part A covers hospital stays, skilled nursing facility care, and some home health services, while Part B covers doctor visits, outpatient care, and preventive services.
- Medicare Advantage (Part C): This is Medicare offered through a private insurance company approved by Medicare. It provides all the benefits of Original Medicare, along with additional coverage for prescription drugs, dental, vision, and hearing services.
- Medicare Supplement (Medigap) plans are designed to fill the gaps in Original Medicare coverage. They help pay for out-of-pocket costs such as deductibles, coinsurance, and copayments. Private insurance companies offer Medigap plans, which are standardized across the states.
- Prescription Drug Plans (Part D): Part D plans are standalone plans offered by private insurance companies. They provide coverage for prescription drugs and can be added to Original Medicare, Medicare Advantage, and some Medicare Cost Plans.
Medicare Plan Comparison Chart
The Medicare Plan Comparisons Chart is a powerful tool that allows you to compare different Medicare plans side by side. It provides a clear and concise overview of each plan’s coverage details, costs, and additional benefits.
Where Can You Find A Chart?
A public tool is on the Medicare website. Type Medicare.gov in your browser address bar and hit enter. You will be taken to the official Medicare website. Click on the button for “Find health & drug plans.” You can create your own account or just type in your zip code without creating an account.
Choose the type of plans you wish to compare: Medicare Advantage Plan (Part C), Medicare drug plan (Part D), or Medigap policy.
Click the button that applies to your situation. Do you get financial help with your plan or not? If you qualify, financial help would be from Nebraska or Iowa Medicaid. Have you qualified for EXTRA HELP? Click Next.
Prescription Drug Comparison
The tool will ask if you wish to include drug costs—type in the specific medications with the dosages.
You may use various filters, but before that, scroll down and look at the plans first. You can look at each plan individually and study the benefits and pricing. There is also a box to check “Add to compare” to examine the plans side-by-side. You are limited to 3 plans at a time.
At the bottom of the screen, you can see the plans’ names and a comparison button. Click the comparison button to bring them up on the screen. The plans will be placed side by side, and all the categories will be matched up between them.
You can see the similarities and differences between the plans in one place and make your determinations. The limitation is that the Medicare.gov software does not provide great detail about the plans individually or together.
At Omaha Insurance Solutions we use a propriety software that goes into much greater detail about each plan. You can see the most common medical plan details: doctor & specialist visits, inpatient & outpatient surgeries, skilled nursing stays, MRIs, and X-rays, etc., compared side-by-side and line by line. Medications are calculated in various totals and subtotals. The provider network search tool is right there to access and find out if your doctors are in the plan or not. We run hundreds of these Medicare plan comparison charts each year for the Medicare plans in the Omaha, Lincoln, & Council Bluffs areas. Contact us for a FREE comparison at 402-614-3389.
Medicare Plan Comparison Chart Interpretation
How do you interpret and analyze the information in front of you? Information can be overwhelming when there is a lot of it, and it is new and unfamiliar. 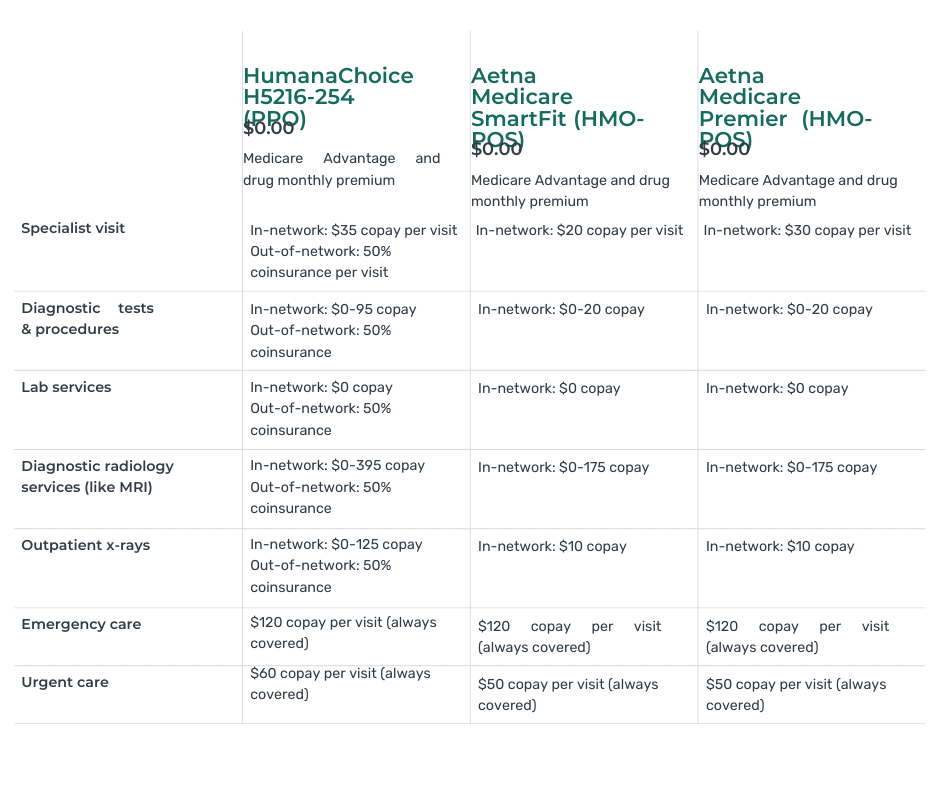
We help clients understand the information and how to weigh the various benefits, particularly in relation to their specific needs and ways of handling their health concerns.
Working with thousands of clients over many years with different health concerns that repeatedly ask many of the same questions, we have learned how to quickly assist you in evaluating and interpreting the information as it is relevant to your needs, situation, and budget.
The chart includes information such as monthly premiums, annual deductibles, coinsurance, copayments, and maximum out-of-pocket costs. It also highlights any limitations or restrictions that may apply to a plan.
By using the chart, you can quickly identify which plans offer the specific coverage you need. For example, if you require prescription drug coverage, you can quickly identify the plans that include Part D that cover your prescriptions at the most affordable prices. If you frequently travel and need coverage outside your local area, you can find plans that offer nationwide coverage.
Key Factors to Consider When Choosing a Medicare Plan
When comparing Medicare plans, there are several key factors to consider. These factors help you determine which plan best suits your needs and preferences. Here are some important considerations:
- Coverage: Evaluate each plan’s coverage options. Consider your existing health conditions and any specific treatments or services you anticipate needing in the future.
- Cost: Compare the costs associated with each plan, including premiums, deductibles, coinsurance, and copayments. Consider your budget and how much you can afford to pay for healthcare services.
- Provider Network: Check whether your preferred healthcare providers, such as doctors and hospitals, are included in the plan’s network. This ensures that you can continue receiving care from your trusted providers.
- Prescription Drug Coverage: If you take prescription medications, ensure the plan offers comprehensive coverage for the needed drugs. Review the formulary to see if your medications are included and at what cost.
- Additional benefits: Some Medicare plans offer additional benefits such as dental, vision, hearing coverage, OTC (Over-the-Counter) items, free gym memberships, and transportation. Consider whether these benefits are important to you and, whether they justify the additional cost, and which provide the maximum coverage.
How to Use the Medicare Plan Comparisons Chart Effectively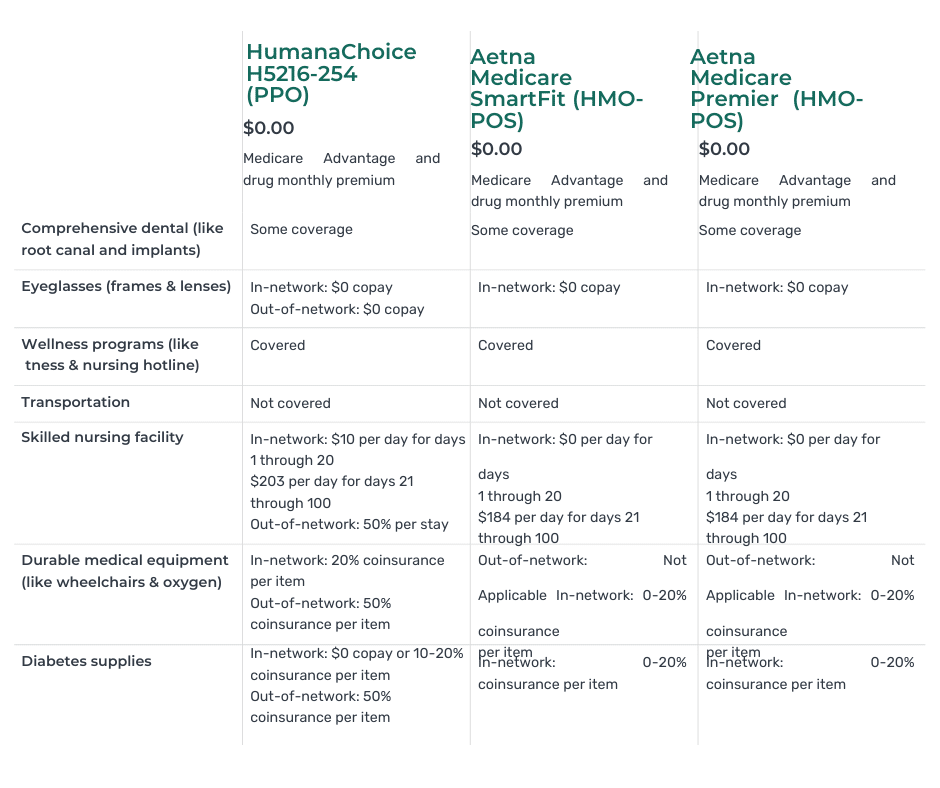
The Medicare Plan Comparisons Chart is designed to simplify choosing a Medicare plan. Here are some tips on how to use the chart effectively:
- Identify your healthcare needs: Before using the chart, take some time to assess your healthcare needs. Consider factors such as existing health conditions, prescription medications, and any specific treatments or services you anticipate needing in the future. This will help you narrow your options and focus on the plans that meet your requirements.
- Focus on relevant information: The chart provides detailed information about each Medicare plan, including coverage details, costs, and additional benefits. Focus on the information that is most relevant to your needs. For example, if you require prescription drug coverage, pay close attention to the details of Part D plans.
- Compare side by side: One of the greatest advantages of the chart is that it allows you to compare different plans side by side. This enables you to evaluate their features and benefits in a clear and concise manner. Take advantage of this feature to identify the plans that offer the specific coverage you need.
- Consider the cost: While coverage is necessary, it’s also essential to consider the cost associated with each plan. Evaluate factors such as monthly premiums, deductibles, copayments, and coinsurance. Consider your budget and how much you can afford to pay for healthcare services.
- Seek assistance if needed: If you find the process overwhelming or have specific questions about the chart or Medicare plans, don’t hesitate to seek assistance. Reach out to a licensed insurance agent or contact Medicare directly for guidance. Making an informed decision based on accurate and up-to-date information is important.
 Bottom Line: Finding the Best Medicare Plan for Your Needs
Bottom Line: Finding the Best Medicare Plan for Your Needs
Choosing the best Medicare plan for your needs is a crucial decision that directly impacts your healthcare coverage and bank account. With the help of the Medicare Plan Comparisons Chart, you can simplify this process and make an informed decision based on your unique healthcare needs.
By understanding the different types of Medicare plans, comparing their coverage options, and considering key factors such as cost, provider networks, and additional benefits, you can confidently select the plan that meets your specific requirements.
Remember to utilize the Medicare Plan Comparisons Chart effectively, focusing on relevant information, comparing plans side by side, and considering both coverage and cost. If needed, seek assistance from

Christopher Grimmond
licensed insurance agents, or contact Medicare directly for guidance.
With the right Medicare plan in place, you can enjoy peace of mind, knowing that you have made the best choice for your healthcare coverage. We take people through this process daily. At no cost to you, we will show you the plans in your area that you are eligible for, break down the information on the chart, and match up with your unique needs and concerns. Call us at 402-614-3389 for a free consultation with a licensed insurance professional.
 Are you confused about Medicare Part D health plans? Don’t worry, you’re not alone. Understanding your options can be overwhelming with all the jargon and complex rules. That’s why we’re here to demystify everything for you.
Are you confused about Medicare Part D health plans? Don’t worry, you’re not alone. Understanding your options can be overwhelming with all the jargon and complex rules. That’s why we’re here to demystify everything for you.
Whether you’re new to Medicare or have been enrolled for years, this article is designed to help you understand the key aspects of Part D plans, including what they cover, how they work, and how to choose the right plan for your needs.
We’ll also answer common questions, such as what medications are covered, how to find the most cost-effective plan, and how to navigate the dreaded coverage gap, known as the “donut hole.”
So, if you’re ready to tackle the confusion surrounding Medicare Part D health plans and take control of your healthcare, let’s dive in and get started.
Who is Eligible for Part D?
Medicare Part D is a prescription drug coverage program the federal government offers to Medicare beneficiaries. Before 2006, there were no government-sponsored prescription drug plans, and the cost of medications was becoming overwhelming for seniors. The Bush Administration introduced a partnership between Medicare and insurance companies known as Part D.
To be eligible for Medicare Part D, you must be enrolled in either Medicare Part A OR Part B. Part A covers hospital stays, while Part B covers doctor visits and outpatient services, but enrollment in either makes you eligible for the Medicare Part D prescription drug benefit.
Medicare Part D health plans are offered by private insurance companies approved by Medicare. These plans are available as standalone prescription drug plans (PDPs) or as part of a Medicare Advantage plan (Part C), which offer additional benefits beyond prescription drug coverage. You must have both Part A and Part B to be eligible for Part C.
 Coverage Options and Costs Under Medicare Part D Health Plans
Coverage Options and Costs Under Medicare Part D Health Plans
Medicare Part D plans provide coverage for a wide range of prescription medications. Each plan has its own formulary, which is a list of covered drugs. Medicare regulations require the plan to have at least two drugs in each of the categories CMS (Center for Medicare & Medicaid Services) specifies. These formularies are divided into tiers, each with a different cost-sharing structure.
The costs associated with Medicare Part D plans can vary depending on your chosen plan. Several components to consider include the monthly premium, annual deductible, copayments or coinsurance, and coverage gap.
Premiums for Part D plans can vary widely, so it’s vital to compare plans to find one that fits your budget. In addition to the premium, many plans have an annual deductible that you must meet before many drug copays work. Once you’ve met the deductible, you’ll typically pay a copayment or coinsurance for each prescription.
It’s also important to be aware of the coverage gap, also known as the “donut hole.” The gap occurs when you reach a specific spending limit; then, your prescription drug costs increase significantly in many cases. However, the coverage gap is gradually closing, thanks to the Inflation Reduction Act legislation.
How to Choose the Right Medicare Part D Health Plan in Your Area
Choosing the right Medicare Part D plan can seem daunting, but with careful consideration, you can find a plan that meets your needs and budget. Here are some factors to consider when comparing plans:
- Coverage: Look for a plan that covers all essential medications. Each plan has its own formulary, so it’s important to review the list of covered drugs to ensure your prescriptions are included.
- Costs: Consider the monthly premium, annual deductible, copayments or coinsurance, and the coverage gap. Calculate how much you would pay out-of-pocket for your medications under each plan to determine which one offers the best value. The total cost is the critical comparison.
- Network: Check if your preferred pharmacies are in the plan’s network. Some plans have preferred pharmacies where you can get lower copayments or coinsurance.
When we run client’s medications, I am still amazed by the difference in cost from one pharmacy to another.
- Plan ratings: The Centers for Medicare and Medicaid Services (CMS) rates Medicare Part D plans on a five-star scale. These ratings can give you an indication of a plan’s quality and customer satisfaction.
By carefully evaluating these factors, you can narrow down your options and choose a Medicare Part D plan that best fits your needs.
Understanding the Different Tiers and Formularies
Medicare Part D formularies are divided into tiers, with each tier representing a different level of cost-sharing. The exact number of tiers can vary depending on the plan, but most plans have at least four tiers.
Tier 1 typically includes generic drugs and has the lowest cost-sharing. Tier 2 includes more expensive but still generic low-cost drugs. Tier 3 is for preferred brand-name drugs, followed by Tier 4 for non-preferred brand-name drugs. Tier 5 is usually reserved for specialty medications, with higher cost-sharing.
It’s important to note that not all drugs are covered on every plan’s formulary, and the specific drugs included in each tier can vary. Before enrolling in a Part D plan, reviewing the formulary to ensure your medications are covered and understanding the associated cost-sharing for each tier is essential.
 My Experience with Medicare Part D Health Plans in Nebraska & Iowa
My Experience with Medicare Part D Health Plans in Nebraska & Iowa
We have over 2,000 Medicare clients at Omaha Insurance Solutions. During the Medicare Annual Election Period (Oct 15th—Dec 7th), we offer an annual review of clients’ plans, especially the medication part of their Medicare plan. Consequently, we run the medications for hundreds of clients through our Medicare Part D health plan software. It performs thousands of calculations and shows the plans in order of least expensive to most for overall cost. The numbers are broken down into various totals and subtotals by months and tiers for premiums and copays.
We put all the data on a big 42-inch screen for the clients to view. The software can easily manipulate the data, so clients can see which plans work best for their mix of medications, which pharmacies give the best pricing, and when and how much they may fall in the Medicare Gap (or “Donut Hole”) over the course of the year, if at all.
You quickly notice patterns after running thousands of simulations of Medicare Part D health plans during Annual Election Period in Nebraska and Iowa. You notice the same four or five plans at the top. Certain pharmacies consistently perform better for certain plans. You see the big differences in which insurance companies and plans are the winners in the new year compared to the previous year. Some inexpensive drugs are no longer covered under certain plans, or the price charged is totally out of proportion to the actual cost. From our experience of running our Part D analysis software for many years and for so many people, we quickly recognize patterns and can advise clients accordingly.
Tips for Saving on Medicare Part D
Prescription drug costs can add up quickly, but there are several strategies you can use to save money with your Medicare Part D plan. Here are some tips to consider:
- Generic drugs: Whenever possible, opt for generic medications. Generic drugs are just as effective as brand-name drugs but are often significantly cheaper.
- Mail-order pharmacy: Some Part D plans offer discounts for using a mail-order pharmacy. Mail-order can be a convenient and cost-effective way to get your medications delivered to your door.
- Medication reviews: Review your medications with your doctor or pharmacist to ensure you’re still taking the most appropriate and cost-effective drugs. They can also identify any potential drug interactions or duplications.
- Extra Help program: If you have limited income and resources, you may qualify for the Extra Help program, which helps cover the costs of prescription drugs.
By implementing these strategies, you can maximize your savings and ensure you get the most value from your Medicare Part D plan.
Common Misconceptions about Medicare Part D
Several common misconceptions surrounding Medicare Part D can lead to confusion and misinformation. Let’s debunk some of these myths:
- Myth: Medicare Part D covers all prescription drugs. Reality: Part D plans have formularies that only cover certain drugs. It’s crucial to review the formulary to ensure your medications are covered.
- Myth: You can switch plans anytime. Reality: You can only switch plans during the annual enrollment period or if you qualify for a special enrollment period.
- Myth: All Part D plans have the same costs and coverage. Reality: Part D plans can vary in terms of premiums, deductibles, copayments, and formularies. It’s important to compare plans to find the best fit.
- Myth: Medicare Part D health plans do not change much from year to year. Reality: Part D plans change, and in some cases, they change a lot.
By understanding these misconceptions, you can make more informed decisions about your Medicare Part D coverage.
Enrolling in a Medicare Part D Plan

Initial Enrollment Period
Enrolling in a Medicare Part D plan is relatively straightforward, but there are specific enrollment periods to be aware of. The Initial Enrollment Period (IEP) is the seven months surrounding your 65th birthday, including the three months before, the month of, and the months after your birthday.
Annual Enrollment Period
If you miss your IEP, you can enroll during the Annual Enrollment Period (AEP), which runs from October 15th to December 7th each year. During this period, you can switch plans or join a Part D plan for the first time.
Special Enrollment Periods
Special Enrollment Periods (SEPs) allow you to enroll outside the IEP or AEP if you experience certain qualifying events. There are many SEP types. One that is very common is when clients move out of their plan’s service area. Clients move and then call us because they have problems getting medications. “Yes, Medicare canceled your plan when you moved out of the area.”
To enroll in a Medicare Part D plan, contact the plans directly, call 1-800-MEDICARE, or call your agent.
If you call an insurance company, they will tell you one of their plans is best for you. They cannot see or sell you the other insurance companies and their plans.
The people you speak with at Medicare don’t work with insurance companies or Medicare plans. They don’t know the plans or how they work. It is like talking to a person who never worked on a car engine, and his only knowledge is from reading a manual and looking at diagrams.
They run the medications you give them through the software. Whatever the software tells them is what they tell you. They have no experience because they have no clients and get no feedback on the advice they are dispensing. There are no consequences to them if they give bad advice. They will never talk to the same person again. They can recommend anything without being held responsible for the advice dispensed. Insurance agents can be held responsible and are.
The Only Way to Get the Information to Make A Truly Informed Choice
I highly recommend working with a trusted and experienced insurance professional who is independent. In other words, an independent agent or broker can show you most or all of the Medicare Part D health plans in your area and the Medicare Advantage plans with prescription drugs. You want to be confident in the person’s knowledge and expertise. Almost anyone can get an insurance license. The person you use should demonstrate knowledge and expertise to you about Medicare and the various insurance plans. They should display reliability. Those are the people to trust. Think about how you pick a doctor.
All Medicare Part D Health Plans and Advantage Plans Are Local
Plans vary from state to state and region to region. At Omaha Insurance Solutions, we are intimately acquainted with the 21 Medicare Part D plans in Nebraska & Iowa, the 30 Medicare Advantage plans in Nebraska, and the 25 Medicare Advantage plans in Iowa. Clients give us daily feedback on how well or poorly the various companies and plans are performing at any given time. We are familiar with our local networks–CHI Health, Nebraska Medicine, Methodist Health Systems, and Bryan Hospital–and other providers. My home is down the street from MD West One. I have had multiple surgeries myself at OrthoNebraska. We know well the Medicare Advantage and Part D plans in Omaha, Lincoln, and Council Bluffs and the doctors and institutions that work with them.
Nebraska, and the 25 Medicare Advantage plans in Iowa. Clients give us daily feedback on how well or poorly the various companies and plans are performing at any given time. We are familiar with our local networks–CHI Health, Nebraska Medicine, Methodist Health Systems, and Bryan Hospital–and other providers. My home is down the street from MD West One. I have had multiple surgeries myself at OrthoNebraska. We know well the Medicare Advantage and Part D plans in Omaha, Lincoln, and Council Bluffs and the doctors and institutions that work with them.
Clients often call us asking for help navigating the customer service bureaucracy when they encounter problems. We constantly hear what is working and not with Medicare Part D health plans in the Omaha, Lincoln, and Council Bluffs areas. We do three-way phone calls with the insurance provider, the pharmacies, and clients to get problems solved. Sometimes, we connect the billing departments of one of the networks with the insurance company and make sure they are communicating correctly so a client is not billed incorrectly.
Unlike the SHIP office or other volunteer organizations that help seniors with Medicare, we find out directly from clients how well Medicare and the Medicare insurance plans are serving them.
Frequently Asked Questions About Medicare Part D
- Question: What medications are covered under Medicare Part D?
Answer: Part D plans cover a wide range of prescription drugs, including generic and brand-name medications. Each plan has its own formulary, so it is essential to review the list of covered drugs.
- Question: How do I find the most cost-effective Part D plan?
Answer: To find the most cost-effective plan, consider factors such as monthly premiums, deductibles, copayments or coinsurance, and the coverage gap. Use the Medicare Plan Finder tool to compare plans based on your specific medications and needs.
Our propriety software sorts through all the plans in your area, confirm the medications on the formulary, lists the copays and premiums, totals the amounts, and reveals the star rating. I believe the information is presented in a much friendlier format than Medicare’s Plan Finder. We perform the service for FREE. Medicare and the insurance companies compensate the agents.
- Question: What is the coverage gap or “donut hole”?
Answer: The coverage gap temporarily increases prescription drug costs after reaching a certain spending limit. However, it is gradually disappearing.
- Question: Can I get assistance paying for my Medicare Part D plan?
Answer: If you have limited income and resources, you may qualify for the Extra Help program, which provides financial assistance to cover the costs of prescription drugs.
Conclusion: The Importance of Understanding Medicare Part D
Medicare Part D health plans play a crucial role in helping seniors and individuals with disabilities afford their prescription medications. By understanding the in’s and out’s of Part D plans, you can make informed decisions about your healthcare coverage and ensure you get the most value from your plan.

Christopher J. Grimmond, MA, CFP
This guide has given you the knowledge you need to demystify Medicare Part D, from knowing what medications are covered to navigating the different tiers and formularies. Remember to review your options, compare plans, and consider cost-saving strategies to maximize your savings.
Don’t let the confusion surrounding Medicare Part D hold you back from taking control of your healthcare. With the right plan and information, you can confidently navigate the world of Medicare Part D and ensure you have access to the medications you need.
If you want assistance and objective analysis of your area’s Medicare Part D health plans, contact us at [email protected] and 402-614-3389. We will provide you with unbiased and free advice on the Medicare plans that will work for you.
Are you wondering if your Medicare Part D plan covers Xarelto? Well, you’re in the right place! This article will unlock the benefits and examine whether Medicare Part D pays for Xarelto. 
Xarelto is a widely prescribed anticoagulant medication used to prevent blood clots. It is commonly prescribed for conditions such as atrial fibrillation, deep vein thrombosis, and pulmonary embolism. Xarelto is also a very expensive medication. Even with Medicare insurance, the copays are high, especially in the Gap phase of Part D.
Navigating the intricacies of Medicare coverage can add an additional level of complexity and confusion around prescription drugs.
Medicare Part D is a prescription drug plan offered by private insurance companies approved by Medicare. The program aims to provide affordable access to various medications, but not all drugs are covered. That’s why it’s crucial to understand whether Xarelto is included in the formulary of your specific Part D plan.
I have hundreds of Medicare clients on Xarelto. We run our clients’ medications through our proprietary software to determine the lowest-cost drug plans. We want the plans to have at least a 3-star or higher Medicare rating. Xarelto is one of many high-dollar medications we have had to deal with for over a decade. This article will delve into Medicare Part D coverage details and explain how we find plans that cover our clients’ Xarelto and other costly medications. So, let’s start unlocking the benefits of Medicare Part D and discovering if Xarelto is covered under your plan.
 Understanding Xarelto and Its Importance
Understanding Xarelto and Its Importance
Xarelto, also known by its generic name rivaroxaban, is an oral anticoagulant medication that plays a crucial role in preventing blood clots. Blood clots can lead to serious health complications such as stroke, heart attack, or even death. Xarelto works by inhibiting the clotting factors in the blood, reducing the risk of clot formation.
The use of Xarelto is particularly prevalent among individuals with conditions such as atrial fibrillation, deep vein thrombosis, and pulmonary embolism. Atrial fibrillation is an irregular heart rhythm that can increase the risk of blood clots forming in the heart. Deep vein thrombosis occurs when blood clots form in the deep veins of the legs, while pulmonary embolism is a life-threatening condition where a blood clot travels to the lungs.
Given the importance of Xarelto in managing these conditions, individuals must have access to affordable medication. This is where Medicare Part D comes into play, offering coverage for prescription drugs to Medicare beneficiaries. Let’s explore the coverage options under Medicare Part D and how they relate to Xarelto.
Coverage Options Under Medicare Part D
Medicare Part D provides coverage for prescription drugs through private insurance companies that contract with Medicare. There are 21 Medicare Part D plans in the Omaha, Lincoln, and Council metro areas. These plans are designed to offer affordable access to a wide range of medications, including Xarelto. As of the writing of this article (January 2024), all 21 Medicare Part D plans pay for Xarelto. However, it’s important to note that not all Part D plans cover every prescription drug.
These plans are designed to offer affordable access to a wide range of medications, including Xarelto. As of the writing of this article (January 2024), all 21 Medicare Part D plans pay for Xarelto. However, it’s important to note that not all Part D plans cover every prescription drug.
Each Medicare Part D plan has a formulary, which is a list of covered drugs. The formulary is divided into different tiers, each with a different cost-sharing structure. Xarelto may be included in the formulary, but its placement within the tiers can affect how much you must pay out of your pocket.
Typically, Part D plans place drugs in different tiers based on their cost and how they compare to other medications in terms of safety and effectiveness. The lower the tier, the lower your out-of-pocket costs will be. It’s worth noting that the formulary and tier structure can vary between different Part D plans, so reviewing your plan’s specific details is essential to determine if Xarelto is covered and at what cost.
 How to Determine if Xarelto is Covered Under Your Medicare Part D Plan
How to Determine if Xarelto is Covered Under Your Medicare Part D Plan
You have a few options to determine if Xarelto is covered under your specific Medicare Part D plan. The first step is to review the plan’s formulary. You can usually find this information on the plan’s website or request a copy of the formulary from the insurance company.
When reviewing the formulary, look for Xarelto or its generic equivalent, rivaroxaban. Note the tier in which it is placed and the associated cost-sharing requirements. Remember that formularies can change from year to year, so reviewing the most up-to-date information is essential.
Another helpful resource is the Medicare Plan Finder tool the Centers for Medicare & Medicaid Services (CMS) provides. This online tool allows you to enter your zip code, current medications, and dosage information to compare different Part D plans in your area. The tool will provide a list of plans and estimated costs. You will learn whether Xarelto is covered and the monthly costs.
If you prefer a more personalized approach, contact the insurance company directly and speak with a representative. They can provide detailed information about your plan’s coverage for Xarelto, including any prior authorization requirements or restrictions.
We Can Help Unlock Your Part B Benefits
Like Medicare, Omaha Insurance Solutions uses a plan finder tool that reviews all the Part D plans, formularies, and prices. The tool shows the various plans, the drug tiers, the medication cost before the Gap (Donut Hole) and in the Gap (Donut Hole), and the total overall cost combining copays and premiums together. You will have a total annual cost for each plan, so you can compare. We also point out the plan’s Medicare star rating.
We can filter the Part D information in many ways so you can look at the data as it applies to you. Our service is free when you are a client. We do this every year during the Annual Election Period for our clients to ensure they are on the best plan for their medication needs and budget.
Researching and understanding your plan’s coverage for all your medications, including Xarelto, can help you make informed decisions about your healthcare and potentially save you money. But what should you do if your Part D plan does not cover Xarelto? Let’s explore the steps you can take in such a situation.
Steps to take if your plan does not cover Xarelto
If your Medicare Part D plan does not cover Xarelto, don’t panic. You can take several steps to explore alternative options and potentially lower your out-of-pocket costs.
1. Speak with your healthcare provider: Your healthcare provider can help you explore alternative medications covered by your plan or suggest other strategies to manage your condition effectively.
2. Request a formulary exception: Sometimes, your healthcare provider can submit a request to the insurance company for a formulary exception. This request outlines why Xarelto is medically necessary for you and provides supporting documentation. If the exception is approved, the insurance company may cover Xarelto, even if it’s not on the formulary.
3. Consider therapeutic alternatives: Your Part D plan may cover alternative medications within the same class as Xarelto. These medications work similarly to Xarelto and may be suitable for your condition. Your healthcare provider can guide you in exploring these alternatives.
4. Explore patient assistance programs: Pharmaceutical companies often offer patient assistance programs that provide financial assistance or free medication to individuals who meet specific eligibility criteria. Due to its high cost, these programs can be a valuable resource if you need help to afford Xarelto.
5. Review other Part D plans: If Xarelto is essential for your health and well-being, consider switching to a different one during the annual enrollment period, typically from October 15th to December 7th each year. By reviewing other plans, you may find one that covers Xarelto or offers more favorable coverage for your specific needs.
Remember, it’s crucial to consult with your healthcare provider and insurance company before changing your medication regimen or coverage. They can provide personalized guidance based on your specific health condition and insurance coverage.
Alternative options for accessing Xarelto at a lower cost
 If Xarelto is not covered by your Medicare Part D plan or the out-of-pocket costs are prohibitively high, alternative options are available to access Xarelto at a lower cost.
If Xarelto is not covered by your Medicare Part D plan or the out-of-pocket costs are prohibitively high, alternative options are available to access Xarelto at a lower cost.
1. Generic alternatives: Generic versions of Xarelto, known as rivaroxaban, may be cheaper. Generic drugs contain the same active ingredients as their brand-name counterparts and are approved by the FDA as safe and effective. Speak with your healthcare provider and pharmacist to explore whether a generic alternative suits you.
2. Manufacturer discounts and coupons: The pharmaceutical manufacturer may offer discounts or coupons that can help reduce the cost of the medication. These savings programs are often available for eligible individuals who meet specific criteria. Check the manufacturer’s website or discuss these programs with your healthcare provider.
3. Medication assistance programs: Non-profit organizations and foundations may offer medication assistance programs that provide financial support or free medication to individuals in need. These programs often have specific eligibility criteria, so it’s important to research and understand the requirements before applying.
4. Pharmacy discount programs: Some pharmacies, including Xarelto, offer discount programs or savings cards to help lower prescription medication costs. These programs may provide discounts for individuals paying out-of-pocket or even those with insurance coverage.
It’s worth noting that while these alternative options can help reduce the cost of Xarelto, it’s important to discuss them with your healthcare provider and consider their recommendations. They can provide valuable insights based on your specific health condition and medication needs.
Tips for Maximizing your Medicare Part D coverage for Xarelto
To maximize your Medicare Part D coverage for Xarelto, consider the following tips:
1. Review your plan annually: Medicare Part D plans can change their formularies and coverage yearly. Take the time to review your plan’s coverage during the annual enrollment period with your agent to ensure Xarelto is still covered and assess any potential changes in cost-sharing requirements. From October 15th to December 7th, we work around the clock to ensure our clients’ medications are covered in their Part D or Medicare Advantage plan within their budget.
ensure Xarelto is still covered and assess any potential changes in cost-sharing requirements. From October 15th to December 7th, we work around the clock to ensure our clients’ medications are covered in their Part D or Medicare Advantage plan within their budget.
2. Consider the total cost: When evaluating different Part D plans, Don’t solely focus on the monthly premium- this is a very common mistake. Consider the deductible, copayments, and coinsurance, as these factors can significantly impact your out-of-pocket costs for Xarelto.
Total Annual Cost! Not just copays, or t just monthly premiums. Not just the cost outside the donut hole. It is the total annual cost you pay.
3. Utilize preferred pharmacies: Some Part D plans have preferred pharmacy networks to access medications at lower copayments. Check if your plan has a preferred pharmacy network, and consider utilizing these pharmacies to reduce your medication costs. I have had clients save hundreds and
4. Explore mail-order options: Mail-order pharmacies often offer discounted prices for prescription medications, including Xarelto. If your plan allows for mail-order prescriptions, it may be worth considering this option to save on your medication costs.
By staying proactive and informed, you can maximize your Medicare Part D coverage and ensure affordable access to Xarelto.
Common Misconceptions about Medicare Part D Coverage for Xarelto
 There are several common misconceptions about Medicare Part D coverage for Xarelto that are important to address:
There are several common misconceptions about Medicare Part D coverage for Xarelto that are important to address:
1. All Part D plans cover Xarelto: Not all Part D plans cover Xarelto, and its coverage can vary depending on the plan. Review your specific plan’s formulary to determine if Xarelto is covered and at what cost is essential.
2. Coverage is the same across all Part D plans: Xarelto’s coverage and cost-sharing requirements can vary between different Part D plans. It’s crucial to compare the formularies and associated costs of various plans to find one that suits your needs.
3. Once covered, Xarelto will always be covered: Formularies can change annually, and a medication covered in the past may not be covered in the future. Reviewing your plan’s formulary annually during the annual enrollment period is vital to ensure Xarelto is still covered.
This Medicare mistake is the bane of my existence. Some clients do not take the annual review period seriously. They do not send us an updated list of medications. They do not talk with us, and when January comes—and it is too late—they call because a particular medication is not covered or the cost is significantly higher than the previous year.
4. Generic alternatives are always covered: While generic alternatives are often less expensive, they may not be covered by all Part D plans. Reviewing your plan’s formulary is crucial to determine if the generic version of Xarelto is covered.
By dispelling these misconceptions, you can approach your Medicare Part D coverage for Xarelto with a clear understanding of what to expect and how to navigate the system’s complexities.
Resources and Assistance Programs for Xarelto Users
If you need assistance accessing Xarelto or managing the cost of the medication, several resources and assistance programs can provide support:
1. Extra Help/Low-Income Subsidy: The Extra Help program is a federal program that helps individuals with limited income and resources pay for their Medicare prescription drug costs. Eligible individuals can receive assistance with premiums, deductibles, and copayments. To determine if you qualify for Extra Help, contact the Social Security Administration or visit their website.
2. Patient Assistance Programs (PAPs): Pharmaceutical manufacturers often offer patient assistance programs that provide free or low-cost medications to individuals who meet specific eligibility criteria. These programs can be a valuable resource for individuals who cannot afford their medications, including Xarelto. Check the manufacturer’s website or discuss these programs with your healthcare provider.
3. State Pharmaceutical Assistance Programs (SPAPs): Some states have their own pharmaceutical assistance programs that provide financial assistance or low-cost medications to eligible individuals. These programs may have specific eligibility criteria and income limits, so it’s important to research the programs available in your state. Nebraska and Iowa do not have these types of programs.
4. Non-profit organizations and foundations: Various non-profit organizations and foundations provide financial assistance or free medication programs for individuals in need. These programs often have specific eligibility criteria and may focus on particular medical conditions. Research and reach out to relevant organizations to explore potential assistance options.
By leveraging these resources and programs, you can access the support you need to afford Xarelto and manage your health effectively.
Conclusion: Making Informed Decisions about Medicare Part D Coverage for Xarelto
Understanding the complexities of Medicare Part D coverage for Xarelto is essential for individuals who rely on this medication to manage their health conditions effectively. By delving into the details of coverage

Christopher J. Grimmond
options, determining if Xarelto is covered by your specific plan, exploring alternative options, and maximizing your Part D coverage, you can make informed decisions about your healthcare.
Remember to consult with your healthcare provider and insurance agent professional throughout the process to ensure you make decisions that align with your specific health needs. By staying proactive and informed, you can unlock the benefits of Medicare Part D and access the necessary medications, such as Xarelto, at an affordable cost. Give us a call at Omaha Insurance Solutions at 402-614-3389, and we will help unlock the benefits of Medicare Part D for you.
As people age, the value of good health becomes more important than ever. When you had a bad fall in your 40s, it would take a few weeks to recover. Now, a bad fall may result in a hip injury that takes months of recovery, doctor visits, physical therapy, or even surgery. Some must go to skilled nursing facilities to recover. The contrast is stark. Seniors’ health issues increase in frequency and complexity as they age. According to the National Council on Aging, nearly 95% of older adults have at least one chronic condition, and 3 million adults aged 65 or older are treated in emergency rooms due to fall-related injuries every year. So Medicare beneficiaries ask: How long Will Medicare Pay for nursing home care and home health care? 
Navigating the Complexities of Care: Medicare’s Coverage of Long-Term Care, Skilled Nursing Facilities, and Home Health Care
While preventative care is essential–annual physicals, screenings, and regular tests–and “fall-proofing” your home is critical, you must be prepared financially for the costs associated with extensive medical care if and when that occurs. If a health event puts you in a situation requiring special care or costly in-facility admittance, your first question will probably be, “How am I going to pay for this?”
If you are a Medicare recipient, navigating care in a long-term care facility can be complex and confusing. There are so many different types of care – long-term care (LTC), skilled nursing facility (SNF), and home healthcare (HH) – that it’s hard to know how it all works and how much Medicare is willing to pay for each.
My job is to make that journey a whole lot easier. I’ll break down each of these care types and dive into what Medicare will and won’t cover so that you know your options if you’re faced with a health challenge that requires ongoing care.
The Differences: LTC vs. SNF vs. HH
Understanding the different types of care offerings can feel like a full-time job for aging adults. Terms like assisted living facilities, senior living providers, and skilled nursing facilities are often used interchangeably, but the truth is, there are subtle differences in care and what and how much Medicare pays for the different types of “nursing home care.”
The three essential categories of care for seniors are long-term care (LTC), skilled nursing facilities (SNF), and home healthcare (HH). Understanding what each one does and its purpose can be beneficial when it comes time to finding care for your specific situation.
Long Term Care (LTC)
Long-Term Care facilities are the places we think of as “nursing homes.” A person may go to a long-term care facility for several reasons and lengths of stay. Permanent residents generally go to LTC facilities primarily because they can no longer perform the activities of daily living.
The 5 activities of daily living are:
- Feeding
- Dressing
- Personal Hygiene (bathing, brushing teeth, clipping nails, etc.)
- Continence (control of bladder and bowels)
- Toileting
If you struggle with any of the above, a Long-Term Care facility may be the right choice for you.
Staffed with caregivers, such as certified nurse assistants, registered nurses, various types of therapists, and doctors–these facilities focus more on providing meals, custodial care like dressing and feeding, and offering social environments for their patients. While also providing health care, the primary focus is custodial care because residents can no longer perform those functions for themselves, their families cannot care for them, and they cannot afford to provide those services in their own homes economically.
 Skilled Nursing Facility (SNF)
Skilled Nursing Facility (SNF)
Skilled nursing facilities are often in the same physical location as long-term care facilities. The difference comes down to the reason behind your stay. If you need care because of a medical condition – such as a broken hip from a fall, car accident, stroke, or heart attack – then an SNF can provide the medical care you need–intense nursing care, physical therapy, speech pathology. Custodial care, such as feeding or toileting, comes with a stay in the skilled nursing facility, but it is secondary to the primary reason for the stay–intense and daily treatment.
Seniors needing intense physical therapy, speech therapy, occupational therapy, or continuous medical support should reside in Skilled Nursing Facilities until they are recovered, reach a certain level, or plateau. Then you return home, where home healthcare takes over. The nurses, physical & occupational therapists, and speech pathologists come to your home. Eventually, when you have progressed in your recovery and do not need treatment as often, home healthcare stops, and you go to providers’ offices for an appointment.
Home Healthcare (HH)
Home Healthcare providers allow their clients to continue living in the comfort of their homes while providing care. The person still cannot get out and go to appointments easily, so the skilled providers come to you in your home two or three times a week or less, depending upon need. Ideally, in the recovery process, you eventually leave your home and go to their offices to receive treatment until you fully recover. Again, home healthcare does not provide custodial care in the home, except on rare occasions for short periods of time.
Understanding that Medicare is health insurance. It covers and pays for doctors, nurses, tests, hospitals–all the things you associate with medical treatment and recovery. Medicare does not provide custodial care, housekeeping, meal & laundry service, or taxis.
Will Medicare Cover Long-Term Care?
When someone says “long-term care” or “nursing home,” they generally mean the person is residing permanently in a facility because she cannot take care of herself–she cannot perform the 5 activities of daily living. Medicare does not pay for nursing home care. Even when medical necessity requires admittance to a nursing home (skilled nursing facility), the length of stay is capped at 100 days. There are rules around stopping and starting this coverage, coming from a hospital stay, and restarting a stay, but essentially, Medicare will only pay for 100 days per year in a nursing home. And Medicare approval for a stay of that length is rare. Again, Medicare pays for “nursing home” care for purposes of intense but temporary medical treatment.
Will Medicare Cover Skilled Nursing Facilities?
Medicare provides “Skilled Nursing Facilities” coverage, but patients must qualify based on stringent requirements. Medicare will only cover SNF care if all of the following are true:
- You are a recipient of Medicare Part A and have days of coverage remaining in your benefit period.
- A qualifying hospital stay preceded the need for SNF. An inpatient stay of at least 3 consecutive days in the hospital followed by admission into an SNF within 30 days of leaving the hospital is required for coverage.
- A doctor must have ordered inpatient SNF care based on medical necessity.
- Your condition requires skilled care daily.
- You need skilled services for an ongoing condition that was treated during your 3-day hospital stay OR a new condition that started while you were already receiving SNF care for an ongoing condition.
- The services must be reasonable and necessary for the treatment of your condition.
- You obtain care through a Medicare-certified SNF.
Even if you qualify, your stay will not last indefinitely.
How Many Days Will Medicare Pay for Skilled Nursing Care?
After qualifying for SNF care, your progress will be closely monitored for the length of your stay, the care you are receiving, and the above requirements to ensure Medicare will continue providing coverage. At a high level, Medicare will cover up to 100 days of SNF coverage within a single benefit period. Again, approval for that length of stay is rare. Medicare wishes to move you to less costly home healthcare as soon as medically possible.
In those 100 days, Medicare will cover the cost of the following:
- A semi-private room
- Meals
- Skilled nursing care
- Medical social services
- Medications
- Medical supplies and equipment usage
- Ambulance transport when required
- Dietary counseling
- Physical therapy, occupational therapy, and speech-language pathology when required to meet your health goal
It’s important to note that while Medicare will provide coverage for 100 days, you will have to supplement the coverage starting on day 21.
- Days 1 – 20: Medicare will pay the total cost; you pay nothing.
- Days 21 – 100: You pay the daily coinsurance, which can be up to $204 per day in 2024.
- Days 101+: Medicare pays nothing; you incur the total cost of care if you remain.
A detailed breakdown of coverage details can be found in Medicare’s SNF handbook. Medicare does not pay for nursing home care unless it is tied to a treatment program while you are in residence.
Will Medicare Cover Home Health Care?
Home healthcare falls under both Medicare Part A and Part B. Home healthcare is defined as part-time or intermittent skilled care when you are “homebound.” Homebound means you cannot leave your home without assistance. Assistance could be using a walker, wheelchair, crutches, or even a cane. You may need special transportation because of your condition. Your doctor may advise you not to leave your home because of your medical condition. These all constitute reasons Medicare will accept for home healthcare.
The usual services home healthcare provides on a part-time basis are:
- physical therapy
- occupation therapy
- speech-language pathology services
- Injectable osteoporosis drugs
- durable medical equipment
A doctor must certify you need home health care through a face-to-face meeting. You need part-time or intermittent care, which may be up to 8 hours per day but with a maximum of 28 hours per week.
Home Healthcare does not include:
- 24-hour adult day care at home
- Meals delivered to the home
- Homemaker services
- Custodial (or personal) care help.
If you do attend adult day care in a facility, you can still qualify for home healthcare.
Getting the Most from Your Medicare: Which Direction?
 There are two ways for you to receive Medicare: Original Medicare or Medicare Advantage.
There are two ways for you to receive Medicare: Original Medicare or Medicare Advantage.
Original Medicare
Original Medicare is Part A for inpatient hospital stays and Part B for outpatient services and doctor visits. There are no networks for Original Medicare. It is fee-for-service (FFS), which means if the doctor or facility accepts Medicare–accept assignment for Medicare is the proper terminology–then Medicare will reimburse the provider for medically necessary services rendered.
Original Medicare does not include Part D for prescriptions, and Orignal Medicare has big gaps in coverage. A quarter of people purchase some sort of supplemental insurance policy, such as Medigap, to fill in the gaps in coverage.
Medicare Advantage/Part C
The other direction is Medicare Advantage (or Part C). These plans are provided by a private insurance company that is Medicare-approved to provide health coverage that is equal to or better than Original Medicare.
The gaps in coverage are structured differently than Original Medicare. Medicare Advantage plans have a maximum out-of-pocket. Original Medicare does not. For example, the most popular Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs have a maximum out-of-pocket of less than $4,000. Original Medicare, on the other hand, does not have a maximum. The sky is the limit for your out-of-pocket costs.
Medicare Advantage is also built on provider networks. The Omaha, Lincoln, Council Bluffs metro area has four healthcare networks: CHI (Catholic Health Initiative), Nebraska Medicine, Methodist Health Systems, and Bryan Hospital. All these networks work with the Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs. Access to providers is a non-issue for us. In other places and with other Medicare Advantage plans, there can be issues and problems, but not here.
Home healthcare is zero for both Original Medicare and most Medicare Advantage plans.
Skilled nursing is zero for the first 20 days for both. On the 21st day, Original Medicare has a copay of $204 during the potential 100 days of coverage–again with no cap on expenses for Part B. Medicare Advantage plans have copays of various sizes, but the key is a limit to what you could pay– a maximum out-of-pocket.
For those who pay the additional premium for the Medigap plan, the skilled nursing facility copay will usually be covered entirely.
Medicare Part D
Medicare Part D prescription drug plans are another premium. Most Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs include the prescription drug plan and are mostly at zero cost.
Neither Original Medicare with a Medigap plan nor Medicare Advantage provides long-term care, custodial care, housekeeping, or adult day care. They may cover some of these services as incidental to providing skilled nursing care in a facility or home but for short periods.
Alternative Ways to Pay for the Care You Need
In 2021, the average cost of long-term care services ranged from $20,280 to $108,405 annually. These prices are exorbitant, and they’re only going up. As you age, the best thing you can do for your health and your wallet is to ensure you have the coverage you can rely on if you need long-term care. Since Medicare doesn’t pay for many long-term care scenarios–“nursing home care”–knowing your other options for coverage is crucial.
 Private Pay
Private Pay
Although challenging, some people will pay for their nursing home care from their savings and assets. By dipping into retirement accounts, tapping into assets such as property or investments, or simply saving up over their lifetimes, some seniors pay out-of-pocket for all the care they receive. This is rare.
One major benefit to this approach is that LTC facilities often prioritize private pay clients when space is limited. With the looming senior care crisis, this will get even more important in the years to come.
Long-Term Care Insurance
A separate long-term care insurance policy can pay the cost of residing in a long-term care facility. In most scenarios, these policies require that you need help with two or more of the activities of daily living (feeding, dressing, hygiene, continence, and toileting) before they take effect. There are usually elimination periods of 30, 60, 90, and 120 days before a policy will pay. The premiums for these insurance plans are not cheap. As you age, like life insurance, the price goes up and can be beyond the budget of many people. You also need to pass underwriting when you apply for the policy, though it will be guaranteed renewal for the rest of your life, no matter your health, as long as you continue to pay the monthly premium.
Veteran Benefits
If you served in the military, you may qualify for some sort of long-term care benefits from the Department of Veterans Affairs. Eligibility will depend upon length of service, type of service, military-related disabilities, and even income. Then, there may be limited or no facility access in your area. Where there is a facility, availability may be limited in terms of beds. Contact the Department of Veteran Affairs to determine for what you qualify. Access is very limited in Nebraska.
Veterans Affairs. Eligibility will depend upon length of service, type of service, military-related disabilities, and even income. Then, there may be limited or no facility access in your area. Where there is a facility, availability may be limited in terms of beds. Contact the Department of Veteran Affairs to determine for what you qualify. Access is very limited in Nebraska.
Medicaid
Often confused with Medicare, Medicaid is an entirely different health program. It’s partially funded by the federal government but funded and managed by the state.
Medicaid provides low-income seniors with financial help for long-term care. Each state has its own eligibility guidelines, but you’ll need to demonstrate financial need to qualify.
Many times people will tell me that so-in-so is in a “nursing home,” and they pay nothing. That is because all their assets have been depleted, and they are on county assistance. Medicaid is paying the bill, and all their assets are gone or will be upon death. The state takes homes and any other assets to offset the loss to the taxpayer who covers the expense.
 Medicare Does Not Pay for Nursing Home Care: Your Health is in Your Hands
Medicare Does Not Pay for Nursing Home Care: Your Health is in Your Hands
LTC, SNF, and HH are a jungle of terms, regulations, insurance, and costs. It is even confusing for experts. Like figuring out your income tax or finances, consulting an insurance professional will be helpful. You need someone who knows Medicare, Medicare insurance, the CMS rules and regulations, and possesses years of experience dealing with Medicare. He can guide you through the maze of Medicare and help you take your health care into your own hands and plan for the best outcome.
You’re in the right place if you’re unsure where to start. Every week, I spend time helping those on Medicare just like you find the right coverage for their needs. At Omaha Insurance Solutions, we can help you figureout the best direction for you, enroll you in Medicare, choose a plan, and get all the T’s cross and I’s dotted on forms and applications. Each year, we will review your needs and the plans available to maximize your Medicare benefits.

Christopher Grimmond
Get in touch with us today at 402-614-3389 for a free, no-obligation consultation about your Medicare options.
 Is Hospice Care Covered by Medicare?
Is Hospice Care Covered by Medicare?
When a loved one receives a terminal diagnosis, they’re typically given an average of six months to live. The next step is to find a place that can meet those special needs. While this is devastating news, the next logical step is to seek out options regarding hospice care to ensure a comfortable transition as their health continues to decline. Of course, figuring out how to pay for hospice care is part of that step. For those on Medicare, how much does Medicare cover for hospice care?
Understanding Medicare’s Hospice Care Coverage
Medicare, the federal health insurance program for individuals age 65 and over, offers coverage for hospice care under Part A. This coverage is available to eligible beneficiaries who have a terminal illness and have a life expectancy of six months or less. Medicare’s hospice care coverage includes a range of services, such as medical and nursing care, pain management, counseling, and medication.
To be eligible for Medicare hospice care, individuals must also be enrolled in Medicare Part A and have their doctor certify that they have a terminal illness with a life expectancy of six months or less. Additionally, individuals must sign a statement choosing hospice care instead of other Medicare-covered benefits for their terminal illness.
How Does Medicare Pay?
Medicare provides financial assistance for hospice care through its hospice benefit under Part A. Medicare Part A covers medications, medical equipment, nursing care, and counseling. The hospice provider is reimbursed directly by Medicare, and the provider must be Medicare-approved to receive reimbursements from Medicare. Beneficiaries are not responsible for any copays.
medical equipment, nursing care, and counseling. The hospice provider is reimbursed directly by Medicare, and the provider must be Medicare-approved to receive reimbursements from Medicare. Beneficiaries are not responsible for any copays.
Medicare’s payment structure for hospice care is based on a per diem (daily) rate. This means that Medicare pays a fixed amount to the hospice provider for each day that an individual is enrolled in hospice care. The per diem rate varies depending on the level of care provided. There may be higher rates for individuals receiving continuous home care or inpatient respite care.
However, it’s important to note that Medicare’s hospice benefit does not cover room and board in a hospice facility. If a beneficiary chooses to receive hospice care in a hospice facility, they may be responsible for paying the room and board costs out of pocket. Alternatively, if a beneficiary receives hospice care at home, Medicare will cover the cost of necessary medical equipment and supplies.
 Medigap & Medicare Advantage with Hospice Care
Medigap & Medicare Advantage with Hospice Care
Medicare Part A covers everything hospice-related. Patient costs are copays for hospice-covered medications and respite care. The copay for hospice medications is no higher than $5. Medicare Part A covers 95% of respite care for persons who have taken responsibility for the dying patient. The patient would be responsible for 5% of the costs.
If an individual has a Medigap policy, the Medigap policy would cover the hospice medications and the coinsurance for respite care. Medicare Advantage would continue to cover everything as before, but it would not normally cover the hospice medication copay or respite coinsurance payment.
It is important to note that there are many other medical costs for hospice patients during their time–non-hospice doctors, hospital beds, emergency room visits, ambulances, oxygen, walkers & wheelchairs, and other non-hospice medications, etc. These expenses fall under Original Medicare and the Medigap policy or Medicare Advantage. Hospice care does not cover these other medical needs. It is important to understand this fact.
Once time the daughter of a client called me to let me know her mother was going into hospice. One of the hospice workers told her to save money by canceling her Medigap policy. I tried to explain there were other medical costs her mother would incur from doctors and other providers, but she was convinced it was an unnecessary expense. Unfortunately, they don’t find out about their mistaken decisions until after the fact and the bills roll in.
Eligibility Requirements for Medicare Covered Hospice Care
To be eligible for Medicare hospice care, individuals must meet certain requirements. First, they must be enrolled in Medicare Part A, which provides hospital insurance coverage. Second, they must have a terminal illness. Terminal is defined as a life expectancy of six months or less, as certified by their doctor. Finally, they must sign a statement choosing hospice care instead of other Medicare-covered benefits for their terminal illness.
A beneficiary can stop hospice care at any point. They are not obliged to remain in hospice once they sign the statement.
It’s important to note that individuals can still receive Medicare hospice care even if they are enrolled in a Medicare Advantage plan. Medicare Advantage plans are private health insurance plans that provide Medicare benefits. You don’t lose Part A when you enroll in a Medicare Advantage plan. It is Part A that pays for hospice, even when you are enrolled in a Medicare Advantage plan.
How Long Does Medicare Pay for Hospice Care?
Once you are certified at the terminal with approximately six months or less of life expectancy, your doctor may recertify you. There are usually two 90-day periods and then every 60 days. You do not need to recommit to hospice. The doctor determines that you are still terminal with a six-month or less time period to live. You can remain in hospice almost indefinitely if you meet the criteria.
The Bottom Line: How Long Does Medicare Cover Palliative Care?

Christopher Grimmond
A quarter of the Medicare budget each year goes to cover the last year of Medicare beneficiaries’ lives. That is an incredible number. Hospice care is an essential part of Medicare.
The practice of hospice exists to provide comfort and optimal quality of life to individuals approaching the end. Medicare provides peace of mind that medical bills will be paid and that care will be provided uninterrupted. As long as a person continues to be certified for hospice, Medicare will continue to cover hospice care. You can be assured Medicare will be there for them the entire time.
Hospice is a difficult time. I have gone through this with both of my parents and with hundreds of clients. Contact us at Omaha Insurance Solutions to speak with a caring insurance professional about your Medicare needs. We are a call away at 402-614-3389.
Many years ago, I was still new to the Medicare insurance business. I had a few hundred clients but no high-income earners. I knew what Medicare IRMAA was, but I had never met someone subject to the IRMAA tax before Doug. He was an improbable candidate. After many years and thousands of clients later, I am very familiar with IRMAA, and I can tell you what the Medicare IRMAA 2024 schedule is all about.
Don’t Judge A Book by Its Cover
Doug drove up to my office on a loud Harley Davidson hog, his long hair waving in the wind. He was a big dude, and his leathers made him even bigger. I was a little nervous, but we sat down and took care of Medicare business.
Medicare business.
A few months later, when Doug’s Medicare started, I got a distressed phone call. “You said my Medicare premium was going to be this amount. It’s three times that!”
I was befuddled. I got my calculator out but couldn’t figure out why it was so high. Finally, I said, “Your income would have to be unusually high to be charged that much.”
Doug got quiet. “How high?” he asked. The first IRMAA bracket was $85,000 for a single person at the time. Doug guffawed and said, “Hell, my income is way more than that.”
Turns out Doug was not only a retired municipal employee with a pension and Social Security. He was also retired from the military with 20 years of service and a pension. On top of that, he had built up a stock portfolio that kicked out around $30,000 in dividend income a year.
I should have taken the adage, ‘Don’t judge a book by its cover’ more seriously.
Since then, I have always brought up income in my introductory meetings and how income affects Medicare Part B premiums. Zip code or fashion choices are no guarantee of what someone’s income may be.
What Is Medicare IRMAA?
 IRMAA stands for income-related monthly adjustment amount. The government loves acronyms. Medicare IRMAA is a surcharge that high-earners pay for their Medicare Part B monthly premium.
IRMAA stands for income-related monthly adjustment amount. The government loves acronyms. Medicare IRMAA is a surcharge that high-earners pay for their Medicare Part B monthly premium.
Everyone pays a tax for Medicare during their working years. The Medicare tax is included in the FICA (Federal Insurance Contribution Act) you pay and is recorded on your pay stubs. Your Medicare tax is currently 1.45%. It is graduated up for higher earners.
In 1966 when the Medicare program began, the cost to workers was $3 per person per month, which is approximately $30 in today’s dollars. The baby boomers are leaving the workforce in huge numbers currently, so fewer workers are paying the Medicare tax. Medicare tax revenue is dropping like a stone in relation to the number of people collecting.
As Baby Boomers leave the workforce, they enter Medicare. The number of workers paying into Medicare is contracting, and the number taking out of the program is ballooning. Medical expenses are climbing. The current demographics are crushing Medicare’s ability to provide the same level of service as in the past because expenses are outpacing tax revenue.
Medicare Prescription Drug Improvement & Modernization Act
In 2003 Congress passed the Medicare Prescription Drug Improvement and Modernization Act of 2003 (MMA). In the legislation, Congress addressed the coming shortfall in Medicare revenue. Congress’s answer was to raise taxes. The top 7 percent of earners were required to pay more into the program. There are currently 65 million Medicare beneficiaries. The IRMAA tax will affect approximately 4.6 million people out of the 65 million. If you are a politician, it is better to keep 60.4 million voters happy, even at the expense of making 4.6 million unhappy.
Congress’s answer was to raise taxes. The top 7 percent of earners were required to pay more into the program. There are currently 65 million Medicare beneficiaries. The IRMAA tax will affect approximately 4.6 million people out of the 65 million. If you are a politician, it is better to keep 60.4 million voters happy, even at the expense of making 4.6 million unhappy.
A little-known fact is Medicare beneficiaries pay less than 25 percent of the actual Medicare cost. The current Part B premium is only $174.70. That premium covers about a fifth of the actual cost. In the MMA, Congress increased the Part B premium based upon your income. The IRMAA increases the percentage that upper-income Medicare beneficiaries actually pay for their Medicare. Instead of paying only 25 percent of the Medicare cost, IRMAA payors pay for 35, 50, 65, 80, or 85 percent of the actual Medicare cost. The additional revenue the IRMAA tax brings in is allocated to offset Medicare’s budget shortfall.
 How Does the Medicare IRMAA 2024 Schedule Work?
How Does the Medicare IRMAA 2024 Schedule Work?
Medicare IRMAA is a different calculation from the progress income tax rates the IRS uses for federal income tax brackets.
You do not pay a federal income tax rate on everything you make. The federal government divides your taxable income into chunks — also known as tax brackets — and each chunk gets taxed at a progressively higher rate. The beauty of this is that no matter which bracket you’re in, you won’t pay the highest tax rate on your entire income! Only the “chunk” in that bracket. For example, you pay 10% on the first $40,000 of income, 25% on the next $20,000 of income (total of $60,000), and 35% on the next $15,000 of income (total of $75,000).
Me dicare IRMAA 2024 schedule utilizes a “cliff” style of assessment instead. That means if you are just $1 over the cut-off for the next tier of IRMAA, you will pay the higher amount. There are no brackets for each chuck of income like federal income tax and no graduation or progression in the amount you pay. The Medicare 2024 Part B IRMAA premium brackets change when you earn one dollar more above the line.
dicare IRMAA 2024 schedule utilizes a “cliff” style of assessment instead. That means if you are just $1 over the cut-off for the next tier of IRMAA, you will pay the higher amount. There are no brackets for each chuck of income like federal income tax and no graduation or progression in the amount you pay. The Medicare 2024 Part B IRMAA premium brackets change when you earn one dollar more above the line.
What Is Medicare IRMAA Based Upon in 2024?
The IRS and Social Security work with Medicare. Medicare determines your income based on your most recent tax filing. So, for example, you are going on Medicare in 2023. The most recent tax filing was in 2022 for 2021. Usually, IRMAA is based on a two-year lag in your income.
How Is Medicare IRMAA Calculated?
Your adjusted gross income (AGI) determines where you fall in the Medicare IRMAA 2024 schedule. The AGI, however, differs from the MAGI (Modified Adjusted Gross Income) you usually think of when doing your taxes. AGI for IRMAA is a Medicare-specific form of MAGI. It is your AGI with tax-exempt bonds–-both earned and accrued interest–-added back into your income. Interest from U.S. Savings bonds used for higher education is added back. Earned income from working abroad that was not added to gross income is included. MAGI (Modified Adjusted Gross Income) for Medicare differs from what MAGI usually means for non-healthcare-related purposes.
You will be sent your Medicare IRMAA Initial Determination Notice soon after you enroll in Medicare Part B. Confirm the income amounts the IRS uses are correct–they make mistakes, too.
 Medicare Financial Planning
Medicare Financial Planning
Examine the Medicare IRMAA 2024 schedule to see if you are close to any of the limits.
What are your plans for the future? Will you withdraw from retirement savings this year or in future years? A home sale can spike your income when your intention is only to downsize and move to a one-story home. Capital gains from a stock and property sale or other appreciated assets may come back to visit you as an unexpected IRMAA tax.
Any of these actions may increase your income substantially enough to move you into and/or up the IRMAA brackets, requiring you to pay more. Knowing and planning for these events, you can move assets in smaller amounts over time to avoid large spikes in income and, consequently, increases in your income tax and IRMAA Part B premium.
How Do I Reduce Medicare IRMAA?
Charitable donations of cash, appreciated assets, and appreciated stock can reduce your taxable and IRMAA surcharge, as well as contributions to 401ks, IRAs, and other qualified programs. Some minor adjustments may drop you down a bracket and save you some money.
What Is the Medicare IRMAA 2024 Schedule?
Since 2007, some Medicare beneficiaries’ Part B monthly premiums included a surcharge based on income. The Medicare IRMAA for 2024 is in the table below.
|
Individual |
Couple | IRMAA Tax |
Part B Total Monthly Premium |
|
Less than $103,000 |
Less than $206,000 | $0.00 |
$174.70 |
|
$103,000 < $129,000 |
$206,000 < $258,000 | $69.90 |
$244.60 |
|
$129,000 < $161,000 |
$258,000 < $322,000 | $174.70 |
$349.40 |
|
$161,000 < $193,000 |
$322,000 < $386,000 | $279.50 |
$454.20 |
|
$193,000 < $500,000 |
$386,000 < $750,000 | $384.30 |
$559.00 |
|
$500,000 < Greater |
$750,000 < Greater | $419.30 |
$594.00 |
Since 2011, higher-income Medicare beneficiaries have paid a surcharge on top of their Medicare Part D premium. The Medicare IRMAA for 2023 prescription drug plans is in the table below. This does not include premiums for specific Medicare Part D plans, Medicare supplements, or Medicare Part C/Medicare Advantage plans. The totals only reflect Part B premiums and Medicare IRMAA 2023 surcharges.
These IRMAA surcharges for Part D have nothing to do with the Part D Gap (or Donut Hole).
|
Individual |
Couple | IRMAA Tax Part D |
Total Monthly Part B & Part D |
|
Less than $103,000 |
Less than $206,000 | $00.00 |
$174.70 |
|
$103,000 < $129,000 |
$206,000 < $258,000 | $12.90 |
$257.50 |
|
$129,000 < $161,000 |
$258,000 < $322,000 | $33.30 |
$382.70 |
|
$161,000 < $193,000 |
$322,000 < $386,000 | $53.80 |
$580.00 |
|
$193,000 < $500,000 |
$386,000 < $750,000 | $74.20 |
$633.20 |
|
$500,000 < Greater |
$750,000 < Greater | $81.00 |
$675.00 |
The Bottom Line For Medicare IRMAA in 2024
Medicare has rules. Lots of rules, including how much you pay if you are successful in our country. We are about helping you navigate the rules, and in the case of Medicare IRMAA for 2024, make sure you do not

Christopher Grimmond
pay one penny more than is required.
If you fall into one of the Medicare IRMAA brackets, talk with your financial planner and tax consultant about minimizing the damage. Get started positioning assets well before 65 and have a plan to move yourself down the Medicare IRMAA 2024 schedule.
We are licensed and experienced insurance professionals. This may be your first Medicare IRMAA rodeo in 2024. It is not ours at Omaha Insurance Solutions. Give us a call and speak with an experienced & licensed insurance agent professional at 402-614-3389.
Is Medicare health insurance an option for you? Medicare is not a one-and-done choice. Medicare is a journey that is quick and short for some. For others, it takes place over years on a road with many twists and turns. What will your Medicare enrollment path look like for 2024?
The Essential Medicare Enrollment Guide is something to read and re-read as you approach each leg of your Medicare journey. As your situation changes, you will need information from different parts of this pamphlet for the various twists and turns in your path. So, your Medicare journey begins.

Medicare Enrollment in 2024: the Twists and Turns
Are you wondering,
- What is this Medicare thing about?
- How does it work?
- What do I have to do & when do I have to do it?
- What are the costs?
- What about my employer health plan? I plan to continue working.
Get these questions answered in the upcoming pages as you consider Medicare enrollment for 2024.
Medicare Vs. Employer Health Insurance: Which is Better for You?
In the landscape of retirement decisions, a challenge arose in the 1980s when Congress upped the eligibility age for Social Security benefits from 65 to 67. Despite this shift, Medicare eligibility remained at 65, prompting many to defer their retirement until they can enjoy full Social Security benefits at 67.
The issue for those who continue to work is whether they should go on Medicare at age 65 or stay on their employer health plan. The quandary is which is a better deal: Medicare OR my employer-provided health insurance? People are stumped. ‘Which way should I go?’
Many of my clients who stayed on their employer health plan complain that they should have gone on Medicare instead of staying on their employer’s health insurance plan. Medicare would have been better, but they didn’t know it.
Medicare typically costs less and provides more coverage than most employer health plans, but no one explains the difference. They didn’t understand Medicare, the rules, the penalties, and the costs. Medicare was a mystery to them. Consequently, they made misinformed decisions.
Find out what they didn’t know before Medicare enrollment for 2024.
What Is Medicare?
Medicare is a federal health insurance program that Congress created in 1965. Congress designed the program to provide health insurance for those who work in the US and are 65 and older. At the time, there was little access to reliable, low-cost health insurance once you retired and lost employer-provided health insurance.
How Do You Qualify for Medicare?
Work History: You must have worked at least 40 quarters (10 years) and paid FICA (Federal Insurance Contribution Act) payroll taxes.
Age or Disability: Once you turn 65 OR are certified as disabled by the Social Security Administration (SSA) with a 24-month waiting period, you can enroll in Medicare.
Special Cases:
- Medicare also immediately covers those with End-Stage Renal Disease (ESRD), which means kidney failure requiring dialysis.
- Medicare likewise immediately covers those with ALS (Amyotrophic Lateral Sclerosis, also called Lou Gehrig’s Disease).
Most of my clients are 65 and older, but I have a number who are disabled or suffer from ESRD and ALS.
What Is Medicare Part A?
Hospital
Medicare health insurance is divided into two parts–Part A and Part B. Medicare Part A is hospital insurance, but Part A covers more than just inpatient hospital stays.
Skilled Nursing Facility Care
After major medical events, the patient may no longer need the intense care an inpatient hospital stay provides. The patient is in recovery. They may need intravenous drugs, wound care, and daily physical or occupational therapy. These are not services ordinarily provided for prolonged periods in a hospital. Instead, a skilled nursing facility is the perfect setting. Part A pays for Skilled Nursing.
Home Health Care
As a patient recovers, they do not need the same level of intense skilled nursing. The next step is to transition to home health care, which, as the name suggests, takes place in the home.
Home health care is intermittent skilled nursing care in the home. Physical therapists, occupational therapists, and speech pathologists come to your home a few times each week to continue your treatments and recovery. Nurses come to care for and rebandage wounds. Part A pays for home health care.
Hospice Care
Part A covers Hospice care exclusively. Hospice is palliative care, which means specialized medical care to relieve pain and other symptoms of serious illness. The intent of hospice care is not to cure or prolong life but to allow the natural processes to proceed with the greatest amount of dignity and the least amount of discomfort. Medicare Part A pays for the hospice medical staff and medications during this process.
Medicare Late Enrollment Penalty
If you are eligible for Medicare Part A, there is no penalty for not enrolling in Part A when first eligible at 65.
People call me in a panic because they heard about a “Medicare penalty.” Relatives or friends told them they must enroll in Medicare at 65. If they don’t, there will be a huge penalty!
There is NO penalty for NOT enrolling in Part A when you turn 65.
There is a penalty, however, for not enrolling in Part B when NOT an active member of an employer health plan.
Not enrolling in Medicare at 65 or older when not an active participant in an employer group health plan will result in the dreaded Medicare penalty.
Many people, however, do belong to employer health plans, and they do not receive any penalty for delaying their Medicare Part B enrollment.
Why Medicare Enrollment for Part A in 2024?
If there is no penalty for not enrolling, then why bother?
I encourage people to enroll in Medicare Part A when they are eligible, even if they have employer health insurance. The reason is you establish your identity with the Social Security Administration (SSA) and CMS (Center for Medicare & Medicaid Services).
Medicare Enrollment Trouble
Sometimes, clients attempt to enroll in Medicare and discover they are blocked. There are errors with their personal information in the government’s database that result in problems and delays.
- For example, SSA has a different spelling for your name. I had a client who thought he was a Michael all his life. He didn’t know his legal name was “Mike” until he tried to enroll in Medicare.
- I’ve had multiple clients’ Medicare delayed because their birthday was one digit off.
- Social Security still had Billy’s old address even though he had been divorced from his wife for three years. She got the house.
- Another client divorced her husband, married another man, divorced him, and remarried her first husband. SSA had her maiden name as her legal name.
- Places of birth are another hidden gem. Clients think they were born in one city but find out it was in a hospital outside the city limits.
- Those born on military bases overseas present a problem in a completely different class of difficulty.
A delay in enrollment in Medicare may be critical when there is a strict timeline. For example, I have had clients scheduled to lose their health insurance in a few weeks. They need a Medicare number to enroll in a Medicare plan, Medicare drug plan, or Medicare Supplement. We could not process the application because there was no Medicare number.
Until the errors are corrected, Social Security cannot enroll you in Medicare.
I have had clients begin the process as early as Social Security allows, which is three months, and they still did not have Medicare coverage in time. SSA or CMS was backed up. There were mistakes in personal data, and/or documents, like birth certificates, were lost and needed to be resubmitted.
Medicare Enrollment On Time for 2024
Starting Medicare insurance on time is critical because essential prescriptions may need to be filled. Hard to get doctor’s appointments are set, vital surgeries are scheduled, and certain treatments cannot wait. Plans fall apart when Medicare delays enrollment past the expected start date.
vital surgeries are scheduled, and certain treatments cannot wait. Plans fall apart when Medicare delays enrollment past the expected start date.
While these incidents are a small percentage of clients, I guarantee you are stressed when it happens to you. We coach clients across the finish line, and coverage starts on time. But time crunches are uncomfortable.
The added benefit is Medicare Part A acts as a secondary payor on medical bills for the areas Part A covers. In other words, your employer plan pays first, then Medicare Part A may pay the remainder of the bill if it falls within Part A’s purview–inpatient hospital, skilled nursing, home health care, etc.
Enrolled in Medicare Part A & HSA
The exception to enrolling in Part A when first eligible is if you plan to contribute to a health savings account (HSA). You cannot actively participate in an HSA and be enrolled in Part A or Part B. The penalties are severe.
 At Least Enroll in Part A at 65
At Least Enroll in Part A at 65
With the exception of being in an HSA, enrollment in Medicare Part A for 2024, when on an employer health plan, is the intelligent thing to do.
You don’t have to worry about a timeline to get it done because you have employer health coverage. You have plenty of time to fix any problems that may arise without rush or pressure. It’s smart.
When you have Part A and your Medicare number, the process is much easier and quicker when you decide to activate your Medicare Part B later.
Your identity is already established, you have a Medicare (MBI) number, and you have some benefit from Part A coverage. Activating Part B is simply a matter of submitting a couple of SSA forms.
How Early Can You Sign Up for a Medicare Supplement?
Previously, some insurance agents would enroll people in Medicare Supplements as early as six months before their 65th birthday. The aim was to lock down the business before another agent signed them up.
Then Medicare changed the Medicare number from the HICN, which was the Social Security number with a letter, to the MBI, which is a unique Medicare Beneficiary Identifier number. CMS (Center for Medicare & Medicaid Services) will not issue the MBI until 3 months before your 65th birthday.
Some insurance agents, however, still continue to complete Medicare Supplement applications 6 months ahead of time without the MBI in an attempt to lock down the business and discourage other agents. They write in your number on the already signed application. In legalize, it is called materially altering a signed contract.
What Is Medicare Part B?
Medicare Part B is Medicare insurance covering doctor visits and outpatient procedures. Part B pays for medically necessary services in these areas as well as preventative care.
How Do You Pay for Part B Medicare?
Your Medicare Part B health insurance has a monthly premium. You pay your Part B premium in one of three ways.
- SSA will deduct your Part B premium from your monthly Social Security benefit check if you are getting benefits.
- You can use Easy Pay on the gov website. Once you have created your MyMedicare.gov account, you can check bills and medications, get a printed or ordered Medicare card, and set up an automatic ETF deduction from your bank account for your Part B premium through Easy Pay.
- You may request SSA send you a paper bill quarterly.
How Much is Part B?
The Medicare Part B premium changes as medical expenses and Medicare administrative costs increase. The current monthly premium for Medicare enrollment for 2024 is $174.70 (2023-$164.90, 2022-$170.10, 2021-$148.50, 2020-$144.60, 2019-$135.50, 2018-$134.00).
You can see the increasing trend. Your Part B premium increasing cost will probably accelerate with current inflationary pressures.
If you are in the top 4% of income earners, your Medicare Part B and Part D premiums will be higher depending upon your level of income.
Medicare Lifetime Late Enrollment Penalty
If you do not enroll in Medicare Part B when first eligible, you will pay a late enrollment penalty for the rest of your life.
You will also be required to wait until the General Enrollment Period (from January 1st–March 31st) to enroll in Part B. Your coverage will begin the 1st of the month following when you enroll.
A permanent 10% penalty will be added to your Part B premium for every 12 months you were not enrolled when you should have been. The penalty is not a one-time late fee. The penalty lasts for as long as you have Part B.
Medicare Late Enrollment Penalty Waiver
Suppose you actively participate in an employer health insurance plan as good as Medicare or other qualifying health plans. In that case, you may delay your Medicare enrollment for 2024 in Part B indefinitely without penalty.
You will also have an open enrollment period whenever you decide to activate your Medicare Part B at any time after 65 when you are actively covered by employer health insurance.
Many people, unfortunately, are entirely unaware of this exception to the rule. As a matter of fact, insurance agents will take advantage of this rule and omit the exception in their discussions to induce people to meet with them and enroll in a Medicare plan.
When Can I Enroll in Medicare
If you are eligible for Medicare when you turn 65, you can sign up
- 3 months before the month of your 65th birthday,
- The month of your 65th birthday,
- The 3 months following your 65th birthday.
Medicare Initial Enrollment Period
- When you enroll in Medicare months 1-3 before the month you turn 65, your Medicare will start the month you turn 65.
- Medicare will start the following month if you enroll in the month in which you turn 65.
- If you enroll the month after you turn 65, Medicare will start the 1st of the following month. The same is true for the next two months.
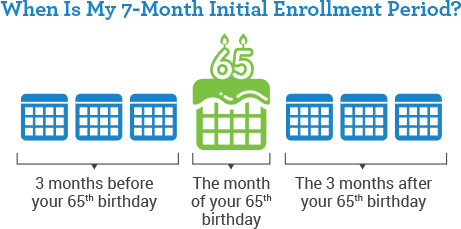
Medicare enrollment for 2024, when you are first eligible, is vital in case of problems. The Social Security Administration (SSA) and Center for Medicare & Medicaid Services (CMS) are slow. Also, there may be errors in your personal information that will require time for correction. Corrections may require supporting documentation, like a birth certificate or naturalization papers. The SSA bureaucratic process does not always function efficiently or quickly. So begin your enrollment process as early as possible.
Part A Post-Dated
After your Initial Enrollment Period (IEP), you may enroll in Medicare Part A anytime. However, Medicare will back-date your Part A six months or to the month you turned 65, whichever is shorter. This rule applies only to Part A.
The six-month back-dating is vital to be aware of if you contribute to an HSA (Health Savings Account). An HSA is attached to an employer’s high-deductible health insurance plan. Medicare has rules and penalties around HSAs. To avoid penalties, you must stop contributing to your HSA at least six months before your Medicare Part A starts if you are older than 65.
First of the Month Birthday
If your 65th birthday is on the first day of the month, your Medicare coverage starts the first of the prior month.
For example, Mr. O’Shea’s 65th birthday is May 1st. His Medicare will start April 1st if he enrolls three months ahead of time–January, February, or March.
Mrs. O’Shea’s 65th birthday is May 2nd. Her Medicare will start May 1st.
 Special Election Period
Special Election Period
Once your Initial Enrollment Period ends, you have another chance for Medicare enrollment for Part B in 2024. This new election period is called a Special Enrollment Period. You need to meet specific criteria for the window of opportunity to open.
Suppose you are covered under an employer health insurance plan that is as good as Medicare. Then, you have a Special Enrollment Period to sign up for Part B as long as you (or your spouse) are working and actively covered by an employer health insurance plan.
You drop your employer health plan and enroll in Medicare. If you are coming off an employer health plan, Medicare will allow you to enroll anytime.
You will not pay a Medicare Part B late enrollment penalty or Part D late enrollment penalty because you had employer health coverage from when you turned 65 until you went on Medicare.
Medicare General Enrollment Period
Suppose you don’t sign up for Part A and/or Part B when you are first eligible and do not qualify for a Special Enrollment Period or have an employer health plan. In that case, you may have to wait until the Medicare General Enrollment Period, which is from January 1st–March 31st.
When you enroll during this Medicare election period, your Medicare will start on the 1st of the following month. For example, you enroll in February. Your Medicare will start on March 1st.
 What is the Medicare Lifetime Late Enrollment Penalty?
What is the Medicare Lifetime Late Enrollment Penalty?
In most cases, you will have to pay a late enrollment penalty for the rest of your life if you sign up during the General Enrollment Period. It means you did not have Medicare Part B and had no employer health insurance plan when you were eligible for Medicare.
The penalty is 10% of the current Part B premium for each full 12-month period you did not have Medicare coverage when you should have.
Yes, if you did not have Part B for five years when you should have and were not an active member of an employer health insurance plan, your late enrollment penalty would result in a 50% surcharge permanently added to your Medicare Part B premium. Not good. That is why it is important to understand your Medicare enrollment requirements for 2024.
When Are You Automatically Enrolled in Medicare?
Suppose you are getting your Social Security (or Railroad Retirement Board) benefits. In that case, you will automatically be enrolled in Medicare Part A and Part B starting the first day of the month you turn 65. If your birthday is on the first day of the month, Part A and Part B will start on the first day of the prior month. You should receive your Medicare card three months before the month of your birthday.
You do not need to do anything if you want to keep Part B. However, if you do not want Part B because you have an employer health plan you prefer, you can cancel Part B by contacting Medicare. The phone number is on the back of the card (800-633-4227), and Medicare is open 24/7.
If you cancel Part B, a new Medicare card will be issued with only Part A on the card. You will always have the option to activate Part B at a later date.
You have the option to purchase a Medicare Part D prescription drug plan with Part A only.
However, if you want to purchase a Medicare Supplement or enroll in a Medicare Part C (Medicare Advantage Plan), Medicare enrollment in Part A and Part B for 2024 is required.
Medicare Due to Disability
Suppose you are eligible for Medicare because of a disability. You will automatically get Part A and Part B after receiving disability benefits from Social Security (or RRB) for 24 months.
Sign up for Medicare But Not Social Security
If you are not currently receiving Social Security (or Railroad Retirement Board) benefits, you must sign up for Medicare Part A and/or B to activate them. You will not automatically receive Medicare benefits like those actively receiving Social Security (or Railroad Board) benefits.
Enrolling In Medicare For the First Time
Social Security is the gatekeeper for Medicare. Signing up for Medicare has evolved over the past few years. The Medicare online enrollment iterations were myriad, but the process is slowly improving and becoming more streamlined.
I happily help my clients enroll in Medicare online weekly.
How Do You Apply For Medicare Online?
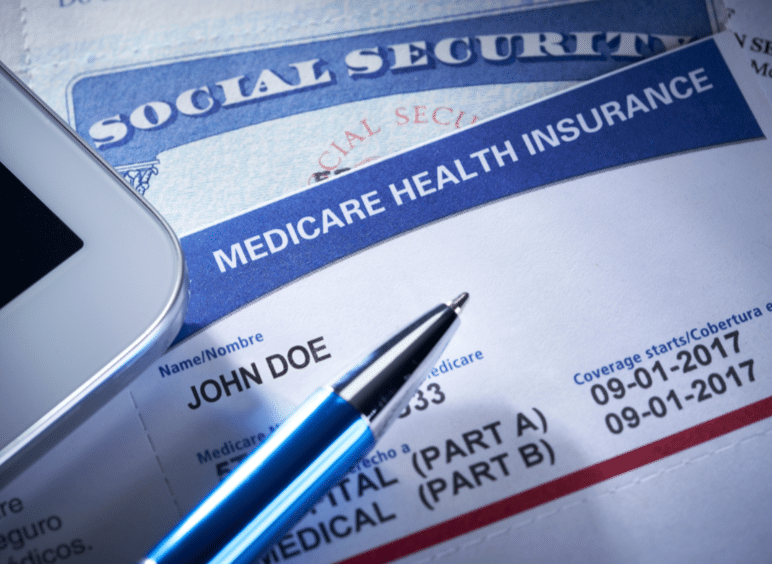 You can call the National Social Security Administration (SSA) at 800-772-1213. I do not recommend that. The hold times are maddening. Do not call Medicare. Medicare cannot enroll you in Medicare. Only SSA can enroll you.
You can call the National Social Security Administration (SSA) at 800-772-1213. I do not recommend that. The hold times are maddening. Do not call Medicare. Medicare cannot enroll you in Medicare. Only SSA can enroll you.
If you are considering Medicare enrollment over the phone for 2024, I suggest calling the local SSA office.
Omaha SSA Office 866-716-8299
Lincoln SSA Office 866-593-2880
Council Bluffs SSA Office 866-331-9094
The local offices will probably set up an appointment many weeks in the future to perform the actual enrollment.
You can also drop by the local office. Prepare to wait or be sent away.
Omaha Address: Old Mill Center 604 N 109th Ct Omaha, NE 68154
Lincoln Address: 100 Centennial Mall N Room 240 Lincoln, NE 68508
Council Bluffs Address: Mid-America Center 20 Arena Way Suite 1 Council Bluffs, IA 51501
The fastest, easiest, and most reliable way to enroll in Medicare is online at the Social Security Administration website (ssa.gov). In the center of the page, under APPLY, click “Sign Up For Medicare.” Follow the prompts.
You will need immediate access to email and text messages to complete the enrollment process. You must have a computer and/or phone with internet, email, and text access to enroll online.
How to Enroll in Part B Medicare
Many people delay enrolling completely in Medicare because they have an employer health insurance plan through work or their spouse’s employer. Several years may pass before they decide to ultimately go on Medicare and leave their employer’s health insurance plan. At some point, however, people retire, quit, or stop working and go entirely on Medicare Part A and Part B.
employer. Several years may pass before they decide to ultimately go on Medicare and leave their employer’s health insurance plan. At some point, however, people retire, quit, or stop working and go entirely on Medicare Part A and Part B.
To enroll in Medicare Part B in this situation, you must complete two CMS (Center for Medicare & Medicaid Services) forms. You will find these forms on the CMS.gov website under forms. The forms are Application for Enrollment in Part B CMS 40B & Request for Employment Information CMS-L564. You can also use the search tool on the CMS.gov website and type “enrollment.”
If you have not enrolled in Medicare Part A by this point, you must also enroll in Part A on the SSA website. Enrolling online for Part A is the preferred method. Calling the SSA office or visiting is usually exceptionally time-consuming. If you already have Medicare Part A, simply complete the two required forms.
Then, fax the two forms to the local Social Security Administration Office.
SSA Omaha Fax: 833-515-0443
SSA Lincoln Fax: 833-641-3167
SSA Council Bluffs Fax: 833-950-2936
Refrain from faxing the forms to the National SSA fax number. I would also mail the forms to the local SSA office. Then, call the local SSA office to confirm the forms were received and processed. If you do all three, you significantly increase the chances of a timely and successful enrollment.
We help our clients do this every day. Our success rate is high when you complete all three steps. Success goes down exponentially when you leave out a step.
 Health Savings Account Contributions & Medicare
Health Savings Account Contributions & Medicare
Once you enroll in Medicare, even if you only enroll in Medicare Part A, you can no longer contribute to an employer’s Health Savings Account (HSA). If you or your employer contributes any amount to your HSA after you enroll in Medicare Part A and/or Part B, you will pay a sizeable tax penalty, and you will need to pay back the unpaid taxes when you withdraw the money from your account.
You must ensure you and your employer stop contributing to your HSA at least six months before your Medicare takes effect if you enroll in Medicare past age 65. Medicare Part A is always back-dated six months (or to your 65th month of birth, whichever is shorter).
Again, do not enroll in either Medicare Part A OR Part B if you wish to continue contributing to an employer HSA.
What is the Medicare HSA Penalty?
The amount of your pre-tax contribution to your HSA during the time you were prohibited will be added back into your past taxable income. You will then be responsible for those past taxes. You will not have the HSA deduction for that period.
An additional 6% amount will also be charged as an IRS penalty accessed on the amount contributed.
 How Do Veteran Benefits Affect Medicare?
How Do Veteran Benefits Affect Medicare?
Many veterans have access to veteran benefits. Veteran benefits are separate from Medicare benefits. The Veteran Administration (VA) administers Veteran benefits. VA benefits are based on the person’s service, time and place of service, disabilities, and even income. Consult the Veteran Administration for your benefits. VA benefits do not affect your Medicare Benefits, though they may work with them. They are two completely separate entities.
Medicare has unique Medicare insurance plans that give additional benefits to veterans who have and use VA benefits. Contact us at 402-614-3389 to speak with a licensed insurance agent professional about these unique plans.
How Does ACA or Marketplace Health Insurance Affect Medicare?
The Health Insurance Marketplace is generally for people who need to buy individual or family health insurance or those offered employer coverage through the Marketplace.
Medicare is not part of the Marketplace. Once you are Medicare eligible and not on an employer health plan, health insurance companies cannot sell you a plan through the Marketplace.
Medicare Vs. Employer Insurance: Which is Better?
Many people continue to work past 65 for various reasons. You can stay on your employer’s health plan or go completely onto Medicare. Medicare is usually better health coverage for the money, but you need to compare.
Four Basic Questions to Ask
To compare Medicare insurance to an employer’s health insurance plan, you need the answer to four questions.
Premium
1.) What is your monthly premium?
If you are on your spouse’s health insurance, your premium may be higher than that of the non-employee.
Deductible
2.) What is the deductible per individual? The deductible is the amount you pay upfront for medical expenses before the plan’s coinsurance pays.
Coinsurance
3.) What is coinsurance? Coinsurance is often a percentage split, like 80% / 20% or 70% / 30%.
Coinsurance is a percentage you pay of the actual cost after you meet the deductible.
For instance, you have a $10,000 medical bill. The deductible is $2,000. After you pay the first $2,000, you then pay 20% on the next $8,000, which is $1,600 of coinsurance. The total between deductible and coinsurance equals $3,600.
Maximum Out-Of-Pocket
4.) The final number is the maximum out-of-pocket (MOOP). The MOOP is the total amount you pay out of your pocket, independent of the insurance company’s payment. You stop paying once you reach your MOOP, and the insurance company pays 100% of the bills from that point on. Your MOOP could be $5,000, $10,000, $15,000, or even higher.
In the above example, if your MOOP is $3,500, you stopped paying at $3,500. If your MOOP were $4,000, you would pay $3,600.
When you have the answers to these four questions, you can compare your employer’s health insurance plan with Medicare and any Medicare plan.
Before Medicare enrollment for 2024, call us at Omaha Insurance Solutions for a free consultation at 402-614-3389 to speak with a licensed insurance agent professional about Medigap, Medicare Advantage, and prescription drug plans and pricing.
 How Do You Weight the Options of Employer Health Insurance Vs. Medicare?
How Do You Weight the Options of Employer Health Insurance Vs. Medicare?
People will often look at the monthly premium to determine which is a better plan. The lower the premium, the better the plan. Premium is undoubtedly a factor among the four, but the deductible is the first consideration when thinking about Medicare enrollment for 2024.
You are eligible for Medicare at age 65. That number is not arbitrary. Even though your health may have been excellent before age 65, health significantly declines in the remaining 18 years, which is the average life expectancy once you reach 65.
Chronic conditions, such as diabetes, arthritis, and heart disease, disproportionally affect those above 65. Eighty percent of Medicare beneficiaries have at least one chronic condition, and nearly 70% have two or more. These conditions worsen with age.
National Poll on Health & Aging
What is the chance you will have outpatient surgery? Elective surgery is more common among adults age 65-80 than adults age 50-64 (36% vs. 25%).
25%).
The five most common elective surgeries Medicare beneficiaries consider are joint surgery (18%), eye surgery (12%), abdominal surgery (10%), cosmetic surgery (9%), and foot or leg surgery (7%).
Those 65-80 were more likely than those age 50-64 to have elective surgery (73% vs. 57%), as were those who were retired or not working compared with those employed (71% vs. 55%). The University of Michigan National Poll on Health & Aging
The Deductible Is Upfront Money
You pay the deductible immediately before the employer’s health insurance begins to cover the surgery. You pay the first $1,000, $2,500, or $5,000 of the $20,000 knee replacement upfront. Then, you pay the coinsurance of 20% for the remaining amount to the maximum out-of-pocket.
The chance that an unforeseen health issue will occur after 65 is significantly higher. The deductible, which is your upfront expense, can instantly wipe out any momentary savings you may have had with a smaller employer health plan premium.
MOOP Is Your Total Risk
The second most important number to consider is the maximum out-of-pocket (MOOP). The MOOP is the most you pay out of your pocket in a year. It is the maximum risk. After reaching that number, the health insurance company will cover your medical expenses 100%. MOOPs are generally large numbers. Paying the MOOP would significantly affect most families’ bottom line.
What is your employer’s health insurance MOOP compared to a Medicare Advantage Plan, Medicare Supplement, and Medicare Part D prescription drug plan? These numbers are usually figured differently, so be careful to make sure you are comparing apples to apples.
When you accurately compare your Medicare options to your current employer’s health insurance plan, you have the essential information to decide.
Will you stay on your employer’s health plan or drop the plan and go completely on Medicare?
 Spouse & Children Are Part of the Equation
Spouse & Children Are Part of the Equation
Other considerations are spouses and perhaps even children. If your spouse, who may be younger, cannot find health insurance from an employer or Marketplace at a reasonable price, and you plan to continue working anyway, remaining on your employer’s health insurance for both of you is likely the better choice. The same is especially true when children are involved.
Where do you find yourself in the Medicare journey? Are you just beginning? Are you still working with only Part A? Is it time to hop on Medicare completely and retire?
A Real Comparison Needs Real Numbers
To make an accurate comparison, you need actual numbers. You need the numbers from your employer’s health insurance plan and the numbers from Medicare, the many Medigap policies, the Part D prescription drug plans, and the Medicare Advantage plans.

Christopher J. Grimmond
We help clients lay out these many plans and numbers in a way that makes sense so you can consider your options and make thoughtful plans and informed choices.
We cost you nothing. The insurance companies and Medicare cover the cost. Our services are FREE. Free means free.
Talk with someone who can interpret the data, explain the information, and evaluate the pricing at Omaha Insurance Solutions. Call us at 402-614-3389 to speak with a licensed insurance agent professional about your Medicare enrollment in 2024.
 Are you looking for comprehensive information on Medicare coverage for Ozempic? Look no further! In this article, we’ll provide everything you need to know about this medication and how Medicare covers it.
Are you looking for comprehensive information on Medicare coverage for Ozempic? Look no further! In this article, we’ll provide everything you need to know about this medication and how Medicare covers it.
Ozempic is a popular prescription medication used to treat type 2 diabetes. It belongs to a class of drugs called GLP-1 receptor agonists, which help lower blood sugar levels and improve overall glycemic control in individuals with diabetes. However, understanding how Medicare covers this medication can sometimes be confusing.
Whether you’re already enrolled in Medicare or planning to do so, it’s crucial to understand the coverage options available for Ozempic clearly. This knowledge can help you make informed decisions about your healthcare and ensure you receive the treatment you need while minimizing out-of-pocket costs.
In this article, we’ll dive into various aspects of Medicare coverage for Ozempic, including the different parts of Medicare, potential costs, coverage criteria, and more. So, if you’re ready to learn about Medicare coverage for Ozempic, let’s get started!
What is Ozempic?
Ozempic is a medication used to treat type 2 diabetes in the class of drugs called GLP-1 receptor agonists, which help lower blood sugar levels. This medication is administered once weekly via injection, making it a convenient option for those managing diabetes. Ozempic is effective in reducing A1C levels and promoting weight loss in patients.
-
How Does Ozempic Work?
Ozempic works by mimicking the action of a naturally occurring hormone called glucagon-like peptide-1 (GLP-1) in the body. GLP-1 helps regulate blood sugar levels by stimulating insulin release, slowing down digestion, and reducing appetite. By activating GLP-1 receptors, Ozempic helps lower blood sugar levels, decrease appetite, and promote weight loss.
body. GLP-1 helps regulate blood sugar levels by stimulating insulin release, slowing down digestion, and reducing appetite. By activating GLP-1 receptors, Ozempic helps lower blood sugar levels, decrease appetite, and promote weight loss.
-
Who Can Benefit from Ozempic?
Ozempic is primarily prescribed to individuals with type 2 diabetes who have not achieved adequate glycemic control through lifestyle changes, such as diet and exercise, or oral diabetes medications alone. It is typically used as an adjunct to diet and exercise to improve blood sugar control.
Like any medication, Ozempic may have potential side effects. Common side effects may include nausea, vomiting, diarrhea, and constipation. These side effects are usually mild and tend to improve over time. However, discussing any concerns or persistent side effects with your healthcare provider is essential.
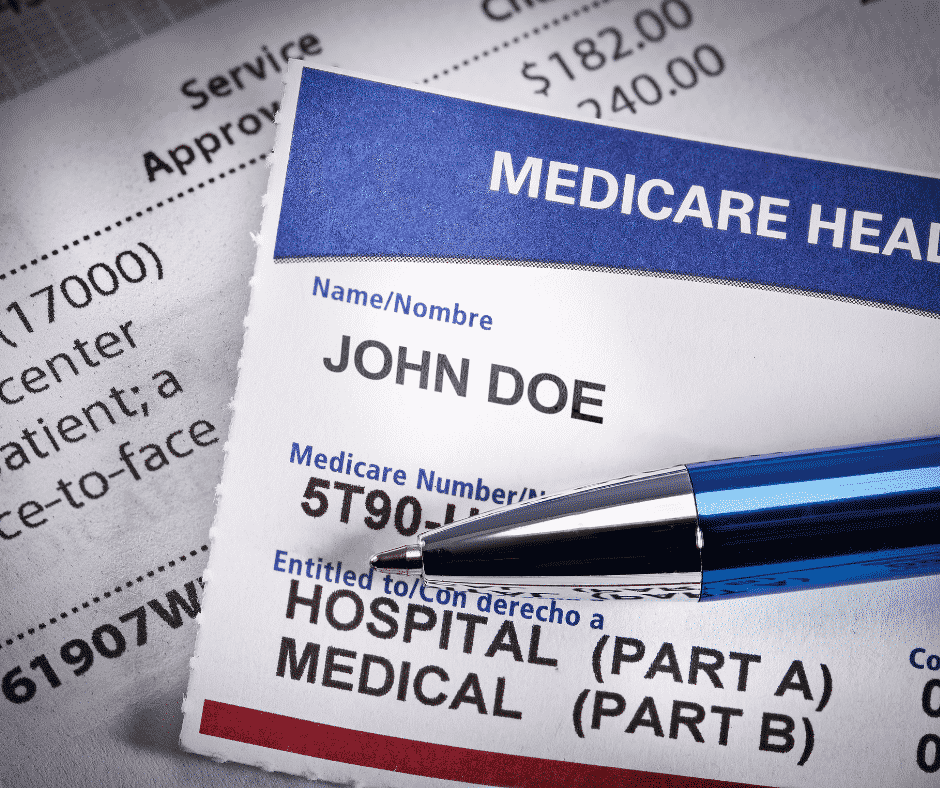 The Importance of Medicare Coverage for Ozempic
The Importance of Medicare Coverage for Ozempic
Understanding Medicare coverage for Ozempic is crucial, especially for individuals with type 2 diabetes who rely on this medication for their health and well-being. Medicare is a federal health insurance program that provides coverage for eligible individuals aged 65 and older, as well as individuals with specific disabilities. Having Medicare coverage for Ozempic can significantly reduce out-of-pocket costs for an expensive medication and ensure access to this essential treatment. According to CMS (Center for Medicare & Medicaid Services), over 459,000 Medicare beneficiaries were on Ozempic, costing CMS over $2.6 billion in 2021.
Understanding Medicare Part D Prescription Drug Coverage
Medicare Part D is the prescription drug coverage portion of Medicare. It is an optional benefit that helps cover the cost of prescription medications, including Ozempic. To receive Medicare Part D coverage, individuals must be enroll in a standalone prescription drug plan (PDP) or a Medicare Advantage plan (Part C) that includes prescription drug coverage.
Private insurance companies approved by Medicare offer Medicare Part D plans. These plans have formularies, which are lists of covered medications. Ozempic is typically included in the formularies of most Medicare Part D plans, but the specific coverage details may vary. It’s essential to review the formulary of the plan you’re considering to ensure Ozempic is covered and to understand any associated costs.
Medicare Part D in the Omaha Metro
 There are 21 Medicare Part D prescription drug plans among seven private insurance companies in the Omaha, Lincoln, and Council Bluffs areas. Seventeen Part D prescription drug plans cover Ozempic. Four do not currently include Ozempic on the formulary. If you are enrolled in those plans, you will have to work with the plan and your doctor for an exception.
There are 21 Medicare Part D prescription drug plans among seven private insurance companies in the Omaha, Lincoln, and Council Bluffs areas. Seventeen Part D prescription drug plans cover Ozempic. Four do not currently include Ozempic on the formulary. If you are enrolled in those plans, you will have to work with the plan and your doctor for an exception.
The plan cost of Ozempic ranges from approximately $800-$950 per month. This amount is used to calculate the levels of cost sharing between the plan and you. This cost-sharing also includes any other medications you are taking. The total will determine how quickly you go from the initial phase, where your Ozempic may cost only $11 to $47 for a month’s supply, to the Gap, when Ozempic may jump to $150–$250, depending upon the plan, excluding your monthly premium for the plan itself.
 Medicare Part C or Medicare Advantage in the Omaha Metro
Medicare Part C or Medicare Advantage in the Omaha Metro
There are 22 Medicare Advantage/Part C plans with prescription drug coverage among six private insurance companies in the Omaha, Lincoln, and Council Bluffs areas. All 21 Advantage plans list Ozempic on their formulary. The plan cost of Ozempic ranges from approximately $890 to $950 per month. This amount is used to calculate the levels of cost sharing between the plan and you. This cost-sharing also includes any other medications you are taking. The total will determine how quickly you go from the initial phase, where your Ozempic may cost only $47 for a month’s supply, to the Gap, when Ozempic may jump to $225–$295, depending upon the plan, excluding your monthly premium for the plan itself if it is not zero.
Eligibility Criteria for Medicare Coverage of Ozempic
 To be eligible for Medicare coverage of Ozempic, you must be enrolled in Medicare Part D or a Medicare Advantage plan that includes prescription drug coverage. Individuals eligible for Medicare Part A and/or Part B are generally eligible for Medicare Part D.
To be eligible for Medicare coverage of Ozempic, you must be enrolled in Medicare Part D or a Medicare Advantage plan that includes prescription drug coverage. Individuals eligible for Medicare Part A and/or Part B are generally eligible for Medicare Part D.
Additionally, Medicare Part D plans may have their own eligibility criteria, such as residence in a specific service area or specific medical conditions. Reviewing the eligibility requirements of the Part D plans in your area is essential to ensure you meet the criteria.
Generally, once your doctor prescripts Ozempic within the standard amounts, the plan will cover Ozempic if it is on the formulary. If it is not on the formulary, you will need to apply for an exception.
Steps to Obtain Medicare Coverage for Ozempic
To obtain Medicare coverage for Ozempic, follow these general steps:
- Enroll in Medicare Part A and/or Part B if you haven’t already done so.
- Decide whether to enroll in a standalone Medicare Part D plan or a Medicare Advantage plan with prescription drug coverage.
- Research and compare Part D plans available in your area to find one that covers Ozempic and meets your healthcare needs.
- Enroll in the Part D plan of your choice during the initial or annual open enrollment period.
- Once enrolled, work with your healthcare provider to obtain a prescription for Ozempic.
- Take your prescription to a pharmacy in-network with your Part D plan and fill your prescription.
It’s important to note that the specific steps and requirements may vary depending on your location and the Part D plan you choose. Consult with Medicare resources or a licensed insurance agent for personalized guidance.
Medicare Coverage Limitations for Ozempic
While Medicare Part D covers Ozempic, certain limitations and cost-sharing requirements may exist. These limitations can include:
- Deductible: Part D plans may have an annual deductible that must be met before coverage begins. The deductible amount varies by plan. The maximum deductible for 2024 is $545. Twelve Part D plans in
 our area out of 21 have a $545 deductible. Three Part D plans have a zero deductible.
our area out of 21 have a $545 deductible. Three Part D plans have a zero deductible. - Copayments or Coinsurance: After meeting the deductible, you may be responsible for copayments or coinsurance for each prescription. The amount will depend on the specific plan and formulary tier Ozempic falls under.
- Quantity Limits: Some Part D plans may impose quantity limits on Ozempic, meaning they will only cover a certain amount per prescription or within a specific time frame.
- Prior Authorization: Certain Part D plans may require prior authorization before covering Ozempic. This means that your healthcare provider will need to provide additional information to the plan to demonstrate medical necessity.
Reviewing the details of your chosen Part D plan to understand any limitations and cost-sharing requirements associated with Ozempic is crucial.
Alternative Options for Obtaining Ozempic
In addition to Medicare Part D coverage, there are alternative options for obtaining Ozempic. These options include:
- Manufacturer Assistance Programs: The manufacturer of Ozempic may offer assistance programs to individuals who meet certain eligibility criteria. These programs can provide financial assistance or free medication to eligible individuals.
- Pharmaceutical Discount Cards: Various pharmaceutical discount cards are available that can help reduce the cost of medications, including Ozempic. These cards are typically free and can be used in addition to Medicare Part D coverage.
- State Pharmaceutical Assistance Programs (SPAPs): Some states offer SPAPs that provide additional prescription drug coverage or financial assistance to eligible individuals. These programs can help lower the cost of Ozempic for those who qualify. Nebraska and Iowa do not have these programs.
- EXTRA HELP is a federal program for those on Medicare to help with medication costs. Assistance depends upon income limits and asset levels.
It’s important to explore these alternative options to ensure you’re taking advantage of all available resources for obtaining Ozempic at an affordable cost.
Additional Resources for Understanding Medicare Coverage for Ozempic
Understanding the intricacies of Medicare coverage for Ozempic can be complex. Fortunately, there are additional resources available to help you navigate this process:
- Medicare.gov: The official Medicare website provides comprehensive information about Medicare coverage options, including Part D and prescription drug coverage. The website provides detailed information, plan comparisons, and enrollment resources.
- State Health Insurance Assistance Programs (SHIPs): Each state has SHIPs that offer free, personalized assistance to Medicare beneficiaries. These programs can guide Medicare coverage options, including Part D, and help you understand how Ozempic is covered in your specific state.
- Licensed Insurance Agents: Working with a licensed insurance agent specializing in Medicare can provide valuable guidance and support. These professionals can help you navigate your area’s various Part D plans and assist with enrollment.
The Bottom Line On Ozempic Medicare Coverage

Christopher Grimmond
Medicare coverage for Ozempic is an important consideration for individuals with type 2 diabetes. Understanding how Medicare Part D works and the potential costs associated with obtaining Ozempic can help ensure you have access to this medication while minimizing out-of-pocket expenses. By utilizing the resources available and exploring alternative options, you can make informed decisions about your healthcare and receive the necessary coverage for Ozempic.
We are a local and independent Medicare insurance agency. Let us find the plan that covers your medications within your budget. We cost you nothing. We charge you nothing. We’re FREE. Call us at 402-614-3389 to speak with a licensed insurance agent professional with over 20 years of insurance experience and over 2,000 Medicare insurance clients. We will get it done right.







